Impaired whole blood thrombin generation is associated with procedure-related bleeding in acutely decompensated cirrhosis.
IF 26.8
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background & Aims
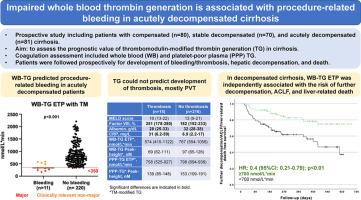
The clinical utility of thrombomodulin-modified thrombin generation (TM-TG) in cirrhosis is uncertain. We conducted a prospective study to evaluate the prognostic value of TM-TG in cirrhosis.Methods
Patients were recruited during outpatient clinics (compensated and stable decompensated) or if admitted to our inpatient service (acutely decompensated, AD). We performed whole blood (WB) and platelet-poor plasma (PPP) TM-TG at recruitment. All patients were prospectively followed-up for bleeding/thrombosis, hepatic decompensation, and liver-related death.Results
We included 231 patients: 80 compensated, 70 stable decompensated, and 81 AD. Median follow-up was 414 days (range: 77-668). Eleven patients, all AD, experienced procedure-related bleeding. Both WB-TG and PPP-TG were more altered in bleeding vs. non-bleeding individuals (lower endogenous thrombin potential [ETP] and peak-height). However, only WB-TG could identify - at individual-patient level - those experiencing major bleeding (all having pre-procedural ETP <350 nmol/L*min). In AD, the area under the ROC curve of WB-TG ETP for bleeding was 0.854 (95%CI: 0.732-0.976), which was higher than that of PPP-TG ETP (0.676; 95%CI: 0.524-0.809). Neither WB-TG nor PPP-TG could predict development of thrombosis, mostly PVT (n=15). In compensated cirrhosis, WB-TG and PPP-TG were comparable between patients who experienced decompensation and those who did not. In decompensated cirrhosis, WB-TG and PPP-TG were more significantly altered in patients experiencing further decompensation/ACLF/liver-related death. A higher WB-TG ETP was linked to a lower risk of progression independently of MELD, Child-Pugh, and C-reactive protein (HR: 0.4, 95%CI: 95%: 0.21-0.79; p<0.01).Conclusions
In compensated cirrhosis, WB-TG and PPP-TG do not improve risk stratification. In decompensated cirrhosis, WB-TG may be a promising tool for estimating procedure-related bleeding risk.Trial registration number
NA
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Hepatology
医学-胃肠肝病学
CiteScore
46.10
自引率
4.30%
发文量
2325
审稿时长
30 days
期刊介绍:
The Journal of Hepatology is the official publication of the European Association for the Study of the Liver (EASL). It is dedicated to presenting clinical and basic research in the field of hepatology through original papers, reviews, case reports, and letters to the Editor. The Journal is published in English and may consider supplements that pass an editorial review.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


