Major Bleeding and Mortality After Revascularization of Left Main Disease
IF 21.7
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
The incidence and prognostic impact of major bleeding (MB) after percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) for left main coronary artery disease (LMCAD) are unknown.
Objectives
The goal of this study was to investigate the rates and outcomes of MB after LMCAD revascularization.
Methods
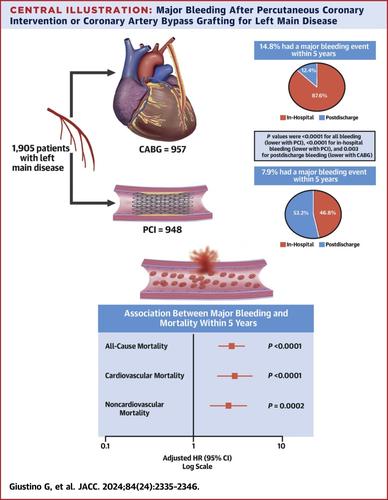
In the EXCEL (Evaluation of XIENCE versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial, 1,905 patients with unprotected LMCAD were randomized to undergo PCI (n = 948) or CABG (n = 957) and followed up for 5 years. MB was defined as TIMI major or minor bleeding, BARC (Bleeding Academic Research Consortium) types 3 to 5 bleeding, or any overt bleeding requiring blood transfusion. The association between MB and subsequent mortality was assessed in time-adjusted Cox regression models.
Results
At 5 years, 217 patients (11.4%) had at least 1 MB event. Rates of 5-year MB were 7.9% after PCI vs 14.8% after CABG (OR: 0.48; 95% CI: 0.36-0.65; P < 0.0001). However, in-hospital MB was lower after PCI (3.8% vs 13.5%; OR: 0.25; 95% CI: 0.17-0.37), whereas postdischarge MB was lower after CABG (4.5% vs 2.0%; OR: 2.33; 95% CI: 1.33-3.09; Pinteraction < 0.0001). All 41 postdischarge MB events after PCI occurred in patients receiving dual antiplatelet therapy. MB events within 5 years were associated with a higher subsequent risk of all-cause mortality (adjusted HR: 2.71; 95% CI: 1.95-3.77; P < 0.0001), whether in-hospital or postdischarge (Pinteraction = 1.00) and after both PCI and CABG (Pinteraction = 0.95), driven both by increased cardiovascular and non-cardiovascular mortality.
Conclusions
In the EXCEL trial, CABG resulted in higher 5-year rates of all MB and in-hospital MB, although postdischarge MB was more frequent after PCI. MB after both procedures was associated with increased cardiovascular and noncardiovascular mortality within 5 years. (Evaluation of XIENCE versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization [EXCEL]; NCT01205776)
左主干疾病血运重建术后大出血与死亡率
背景:经皮冠状动脉介入治疗(PCI)和冠状动脉旁路移植术(CABG)治疗左主干冠状动脉疾病(LMCAD)后大出血(MB)的发生率和预后影响尚不清楚。目的本研究的目的是调查LMCAD血运重建术后MB的发生率和结果。方法在EXCEL (Evaluation of XIENCE vs冠状动脉搭桥手术对左主干血运重建的有效性的评价)试验中,1905例无保护LMCAD患者随机分为PCI (n = 948)和CABG (n = 957)两组,随访5年。MB定义为TIMI大出血或轻度出血,BARC(出血学术研究联盟)3 - 5型出血,或任何需要输血的明显出血。在时间调整的Cox回归模型中评估MB与随后死亡率之间的关系。结果5年内,217例(11.4%)患者至少发生1次MB事件。PCI术后5年MB发生率为7.9%,CABG术后为14.8% (OR: 0.48;95% ci: 0.36-0.65;P & lt;0.0001)。然而,PCI术后住院MB较低(3.8% vs 13.5%;OR: 0.25;95% CI: 0.17-0.37),而CABG术后出院后MB较低(4.5% vs 2.0%;OR: 2.33;95% ci: 1.33-3.09;Pinteraction & lt;0.0001)。所有41例PCI术后MB事件均发生在接受双重抗血小板治疗的患者中。5年内MB事件与随后更高的全因死亡风险相关(调整后风险比:2.71;95% ci: 1.95-3.77;P & lt;0.0001),无论是住院还是出院后(p相互作用= 1.00),以及PCI和CABG后(p相互作用= 0.95),都是由心血管和非心血管死亡率增加引起的。结论在EXCEL试验中,CABG导致所有MB和院内MB的5年发生率较高,尽管PCI术后出院后MB发生率更高。两种手术后的MB与5年内心血管和非心血管死亡率增加有关。XIENCE与冠状动脉搭桥术对左主干血运重建术效果的评价[EXCEL];NCT01205776)
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
42.70
自引率
3.30%
发文量
5097
审稿时长
2-4 weeks
期刊介绍:
The Journal of the American College of Cardiology (JACC) publishes peer-reviewed articles highlighting all aspects of cardiovascular disease, including original clinical studies, experimental investigations with clear clinical relevance, state-of-the-art papers and viewpoints.
Content Profile:
-Original Investigations
-JACC State-of-the-Art Reviews
-JACC Review Topics of the Week
-Guidelines & Clinical Documents
-JACC Guideline Comparisons
-JACC Scientific Expert Panels
-Cardiovascular Medicine & Society
-Editorial Comments (accompanying every Original Investigation)
-Research Letters
-Fellows-in-Training/Early Career Professional Pages
-Editor’s Pages from the Editor-in-Chief or other invited thought leaders

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


