Underestimated risk of secondary complications in pathogenic and glucose-elevating GCK variant carriers with type 2 diabetes
IF 5.4
Q1 MEDICINE, RESEARCH & EXPERIMENTAL
引用次数: 0
Abstract
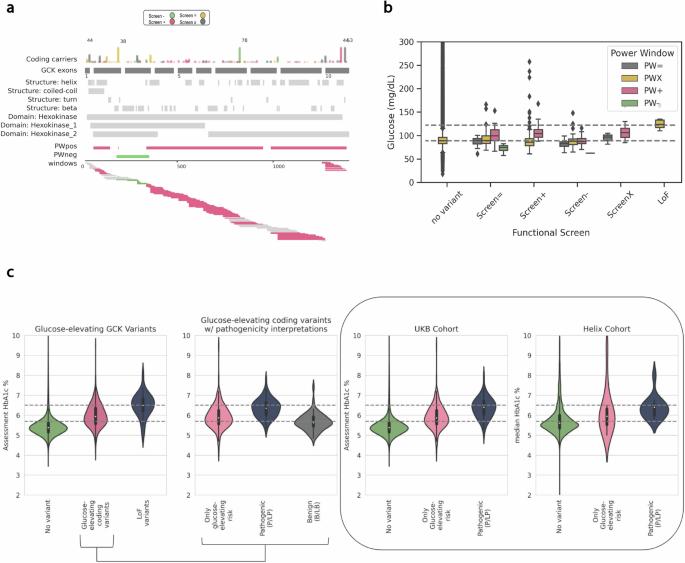
Natural HbA1c levels in GCK Maturity-onset diabetes of the young (GCK-MODY) patients often sit above the diagnostic threshold for type 2 diabetes (T2D). Treatments to lower HbA1c levels show reduced effectiveness in these individuals, yet in case studies to date, GCK-MODY patients often evade secondary T2D complications. Given these deviations, genetic screening of GCK may be clinically useful, but population studies are needed to more broadly understand T2D-related complications in GCK variant carriers. To identify GCK variant carriers at the population level, we used both ACMG/AMP variant interpretation for GCK-MODY pathogenicity and a state-of-the-art variant interpretation strategy based on functional and statistical evidence to predict glucose elevations. Presence of pathogenic and glucose-elevating GCK variants was assessed in two cohorts (n~535,000). We identified 442 individuals with GCK variants predicted to increase glucose (~1/1200), with 150 (34%) of these individuals harboring variants reaching a pathogenic interpretation. In a retrospective analysis, we show that in addition to elevated HbA1c, pathogenic variant carriers are 10x as likely, and all other glucose-elevating GCK variant carriers are 3x as likely, to receive a T2D diagnosis compared to non-GCK carriers. Surprisingly, carriers of pathogenic and glucose-elevating GCK variants with T2D develop T2D-related complications at rates more than double that of individuals without T2D, comparable to non-GCK individuals with T2D. This population-level assessment shows secondary complications in individuals with pathogenic and glucose-elevating GCK variants and T2D and suggests that genotyping for these variants should be considered in a precision medicine approach for T2D treatment and prevention. This study investigates the role of the GCK gene in Type 2 Diabetes (T2D). Variations in the GCK gene are known to cause a form of diabetes that is characterized by early onset and stable blood sugar levels, with a low risk of the type of complications often experienced by people with other causes of T2D. However, our study of a large number of people living in both the United Kingdom and the United States shows that some specific variations in the GCK gene give people a higher risk of developing T2D with the typical secondary complications. This suggests that knowledge of GCK variation in a person should be considered when optimizing T2D prevention and treatment strategies. Schiabor Barrett et al evaluate variants in GCK, a gene associated with Monogenic Diabetes of the Young (MODY), in two population cohorts with healthcare records. They find that participants with pathogenic MODY and other glucose-elevating variants are at risk for Type 2 Diabetes (T2D) and those with T2D show secondary complications of T2D.
低估了致病型和血糖升高型 GCK 变异携带者 2 型糖尿病继发性并发症的风险。
背景:GCK 成熟型青年糖尿病(GCK-MODY)患者的自然 HbA1c 水平往往高于 2 型糖尿病(T2D)的诊断阈值。降低 HbA1c 水平的治疗对这些人的疗效较差,但在迄今为止的个案研究中,GCK-MODY 患者往往能避免继发 T2D 并发症。鉴于这些偏差,GCK 基因筛查可能对临床有用,但还需要进行人群研究,以更广泛地了解 GCK 变异携带者的 T2D 相关并发症:为了在人群水平上识别 GCK 变异携带者,我们同时使用了 ACMG/AMP 变异解释 GCK-MODY 的致病性,以及基于功能和统计证据的最新变异解释策略来预测血糖升高。我们在两个队列(n~535,000)中评估了致病性和血糖升高性 GCK 变异的存在。我们确定了 442 人的 GCK 变异预测会使血糖升高(约为 1/1200),其中 150 人(34%)的变异达到了致病性解释:在一项回顾性分析中,我们发现除了 HbA1c 升高外,与非 GCK 变异携带者相比,致病性变异携带者被诊断为 T2D 的几率是非 GCK 变异携带者的 10 倍,而所有其他血糖升高 GCK 变异携带者被诊断为 T2D 的几率是非 GCK 变异携带者的 3 倍。令人惊讶的是,患有 T2D 的致病性 GCK 变体和葡萄糖升高 GCK 变体携带者患 T2D 相关并发症的比例是无 T2D 患者的两倍多,与患有 T2D 的非 GCK 患者相当:这项人群水平的评估显示,具有致病性和血糖升高GCK变异体的T2D患者会出现继发性并发症,这表明在T2D治疗和预防的精准医学方法中应考虑对这些变异体进行基因分型。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


