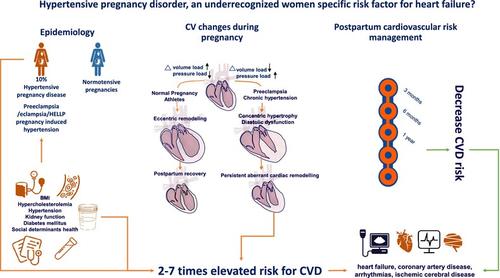
Hypertensive pregnancy disorder, an under-recognized women specific risk factor for heart failure?
IF 16.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
During pregnancy, the maternal cardiovascular (CV) system undergoes major haemodynamic alterations ensuring adequate placental perfusion and a healthy pregnancy course. Hypertensive disorders of pregnancy (HDP) occur in almost 10% of gestations and preeclampsia, a more severe form, in 3–4%. Women with HDP demonstrated impaired myocardial function, biventricular chamber dysfunction and adverse biventricular remodelling. Shortly after delivery, women who experienced HDP express increased risk of classic CV risk factors such as hypertension, renal disease, abnormal lipid profile, and diabetes. Within the first two decades following a HDP, women experience increased rates of heart failure, chronic hypertension, ischaemic heart and cerebral disease. The mechanism underlying the relationship between HDP in younger women and CV disease later in life could be explained by sharing pre-pregnancy CV risk factors or due to a direct impact of HDP on the maternal CV system conferring a state of increased susceptibility to future metabolic or haemodynamic insults. Racial disparities in CV risk and social determinants of health also play an important role in their remote CV risk. Although there is general agreement that women who suffered from HDP should undertake early CV screening to allow appropriate prevention and timely treatment, a screening and intervention protocol has not been standardized due to limited available evidence. In this review, we discuss why women with hypertensive pregnancy may be disproportionately affected by heart failure with preserved ejection fraction and how cardiac remodelling during or after pregnancy may influence its development.
妊娠高血压疾病,一个未被充分认识的女性心力衰竭特异性风险因素?
妊娠期间,母体的心血管(CV)系统会发生重大的血流动力学变化,以确保胎盘有足够的灌注和健康的妊娠过程。妊娠期高血压疾病(HDP)发生率接近 10%,而子痫前期(一种更严重的疾病)发生率为 3-4%。患有 HDP 的妇女心肌功能受损、双心室腔功能障碍和双心室重塑不良。产后不久,经历过 HDP 的妇女出现高血压、肾病、血脂异常和糖尿病等典型心血管风险因素的风险增加。在经历 HDP 后的头二十年内,妇女罹患心力衰竭、慢性高血压、缺血性心脏和脑部疾病的比例会增加。年轻女性 HDP 与日后心血管疾病之间关系的内在机制,可能是由于孕前心血管疾病风险因素的共享,也可能是由于 HDP 对母体心血管系统的直接影响,使其对未来代谢或血流动力学损伤的易感性增加。心血管疾病风险的种族差异和健康的社会决定因素也对她们的远期心血管疾病风险起着重要作用。尽管人们普遍认为,罹患 HDP 的女性应进行早期心血管疾病筛查,以便进行适当的预防和及时的治疗,但由于可用证据有限,筛查和干预方案尚未标准化。在这篇综述中,我们将讨论为什么患有妊娠高血压的妇女会受到射血分数保留型心力衰竭的过度影响,以及妊娠期间或之后的心脏重塑如何影响其发展。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

European Journal of Heart Failure
医学-心血管系统
CiteScore
27.30
自引率
11.50%
发文量
365
审稿时长
1 months
期刊介绍:
European Journal of Heart Failure is an international journal dedicated to advancing knowledge in the field of heart failure management. The journal publishes reviews and editorials aimed at improving understanding, prevention, investigation, and treatment of heart failure. It covers various disciplines such as molecular and cellular biology, pathology, physiology, electrophysiology, pharmacology, clinical sciences, social sciences, and population sciences. The journal welcomes submissions of manuscripts on basic, clinical, and population sciences, as well as original contributions on nursing, care of the elderly, primary care, health economics, and other related specialist fields. It is published monthly and has a readership that includes cardiologists, emergency room physicians, intensivists, internists, general physicians, cardiac nurses, diabetologists, epidemiologists, basic scientists focusing on cardiovascular research, and those working in rehabilitation. The journal is abstracted and indexed in various databases such as Academic Search, Embase, MEDLINE/PubMed, and Science Citation Index.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


