Underrepresentation of women in cardiovascular disease clinical Trials—What’s in a Name?
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
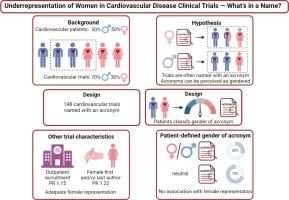
Cardiovascular disease is the leading cause of death in women worldwide. Yet, women are often underrepresented in cardiovascular clinical trials. Trial characteristics may influence the participation of women. For instance, trials are often entitled with an acronym, which might be perceived as gendered. We aimed to investigate if the perceived gender of the acronym and other trial characteristics affect the representation of female patients in cardiovascular trials.
Methods
We searched ClinicalTrials.gov for randomized controlled trials in cardiovascular disease named with an acronym. Cardiovascular patients (n = 148) scored the perceived gender of the acronym of 148 identified trials. Prevalence ratios (PR) were calculated with Poisson regression to link trial characteristics to representation of female patients in the trials.
Results
In 62 % of trials, female patients were underrepresented relative to the disease population. There was no improvement over time in proportion of trials with adequate representation. A third of acronyms was classified as gendered. The perceived gender did not affect representation of female patients (PR 1.01; 95% CI 0.95 – 1.08; P = 0.68). A woman as first and/or last author (PR 1.22; 95% CI 1.07 – 1.38; P = 0.002) and recruitment in an outpatient setting (PR 1.15; 95% CI 1.02 – 1.29; P = 0.01) were associated with a higher prevalence of adequate representation of female patients.
Conclusions
Representation of female patients in cardiovascular trials does not depend on the perceived gender of the trial acronym but is improved in trials under female leadership in out-patient settings. Our findings may direct efforts towards increasing representation of female patients in cardiovascular trials.
心血管疾病临床试验中女性代表人数不足--名称有何意义?
背景心血管疾病是导致全球女性死亡的主要原因。然而,在心血管临床试验中,女性的参与人数往往不足。试验的特点可能会影响女性的参与。例如,试验的名称通常会有一个缩写,这可能会被认为是有性别区分的。我们的目的是调查缩写的性别感知和其他试验特征是否会影响女性患者在心血管试验中的代表性。方法我们在ClinicalTrials.gov中搜索了以缩写命名的心血管疾病随机对照试验。心血管病患者(n = 148)对 148 项已确定试验的首字母缩略词的感知性别进行了评分。通过泊松回归计算患病率比(PR),将试验特征与试验中女性患者的代表性联系起来。随着时间的推移,具有充分代表性的试验比例没有提高。三分之一的缩略词被归类为性别词。认为的性别并不影响女性患者的代表性(PR 1.01;95% CI 0.95 - 1.08;P = 0.68)。女性作为第一作者和/或最后作者(PR 1.22;95% CI 1.07 - 1.38;P = 0.002)以及在门诊环境中招募(PR 1.15;95% CI 1.02 - 1.29;P = 0.01)与女性患者的充分代表性较高相关。我们的研究结果可为提高女性患者在心血管试验中的代表性提供指导。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


