Analysis of genotype resistance and HIV-1 transmission risk in HIV-1-infected men who have sex with men in Guiyang, China
Abstract
Background
As the social economy has developed and population mobility has increased, differences in the Human immunodeficiency virus type 1 (HIV-1) genotype distribution among men who have sex with men (MSM) have become apparent in the provinces and cities across China. The high variability and drug resistance characteristics of HIV-1 can lead to the widespread spread of resistant strains, which may also result in antiretroviral therapy failure and an increase in the mortality rate.
Objective
The genotypic drug resistance characteristics and HIV-1 transmission risks among HIV-1-infected MSM in Guiyang, Guizhou Province were analyzed in the current study. The aim of the study was to provide a scientific basis for preventing the spread of HIV-1 strains among MSM and develop intervention measures.
Method
A cross-sectional study was conducted at the Guiyang Public Health Clinical Center. A total of 181 HIV-1-infected MSM who not received treatment at the center between 1 January 2020 and 31 December 2022 were selected. The HIV-1 pol region gene fragment, including the protease and reverse transcriptase regions, was amplified by nested PCR and RT-PCR. The maximum likelihood method was used to construct a phylogenetic tree for analyzing the HIV-1 genotypes in MSM. HIV-1 genotypic resistance was evaluated using the Stanford University HIV drug resistance database. A molecular transmission network of HIV was constructed and the risk of HIV-1 transmission was determined.
Results
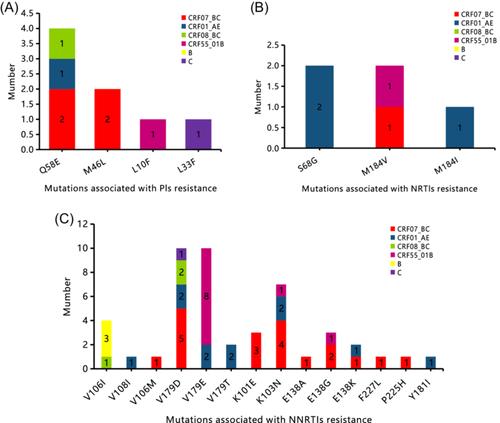
We successfully amplified 173 pol gene sequences from blood samples obtained from 181 patients. The main subtype was CRF07_BC (60.69% [105/173]), followed by CRF01_AE (26.59% [46/173]), CRF08_BC (4.05% [7/173]), CRF55_01B (4.62% [8/173]), B (3.47% [6/173]), and C (0.58% [1/173]). The distribution of HIV-1 genotypes in MSM showed that there was a significant difference in the genotype composition of HIV-1-infected MSM according to registered residences and ages (p < .05). The CRF55_01B subtype accounted for the lowest proportion in Guiyang City and individuals >30 years of age. Multivariate logistic regression analysis of risk factors for drug resistance in HIV-1-infected MSM showed that the overall prevalence of pretreatment drug-resistant species was 12.72% (22/173), and age >30 years, CRF55_01B subtype, and CD4+ T lymphocyte count >350 cells/mm3 were risk factors for drug resistance in MSM HIV-1 strains. Among the pretreatment drug-resistant species, non-nucleoside reverse transcriptase inhibitors with ≥1 drug resistant-species accounted for 9.25% (16/173), followed by protease inhibitors at 4.05% (7/173) and nucleoside reverse transcriptase inhibitors at 1.73% (3/173). Non-nucleoside reverse transcriptase inhibitors resistant to the CRF07_BC and CRF01_AE genotypes were predominant. The CRF55_01B genotype was shown to be most likely to carry the V179E mutation. The molecular network included CRF07_BC and B genotypes. The results of multi-factor logistic regression analysis on the factors affecting the rate of joining the network showed that individuals >30 years of age were less likely to join the network compared to those individuals <30 years of age.
Conclusion
The distribution of HIV-1 genotypes among MSM in Guiyang is diverse and complex. The main genotypes were shown to be CRF07_BC and CRF01_AE. The drug resistance mutation rate is high and pretreatment drug-resistant species is at a moderate level of prevalence, with NNRTIs being the most common site for drug resistance mutations. The CRF07_BC subtype and patients <30 years of age were identified as the key intervention targets in Guiyang based on the molecular transmission network. Patients should routinely undergo drug resistance testing before starting antiretroviral therapy to avoid virologic treatment failure and prevent the spread of HIV-1-resistant strains in MSM.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


