Delivery of Supported Self-Management in Primary Care Asthma Reviews: Insights From the IMP2ART Programme
Abstract
Background
Supported self-management (SSM) for asthma reduces the risk of asthma attacks and improves asthma control and quality of life. SSM optimally includes patient-centred communication and behaviour change support, however, the extent to which this occurs in routine primary care is unclear. This project was nested within the IMPlementing IMProved Asthma self-management as RouTine (IMP2ART) programme; a UK-wide trial evaluating an implementation strategy (including healthcare professional (HCP) training on behaviour change strategies and patient-centred care) to improve support for asthma self-management.
Objective
To provide an understanding of how healthcare professionals deliver SSM in UK clinical practice; through assessing time spent on SSM strategies, how and to what extent patient-centred care and behaviour change discussions are delivered, and to explore whether factors such as mode of review or implementation support influence delivery.
Design, Setting and Participants
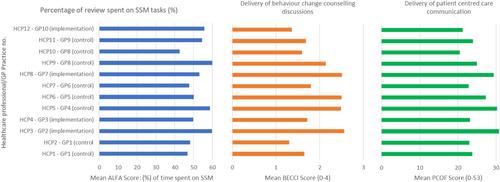
We conducted an observational study using video-recordings of 12 HCPs delivering routine face-to-face and telephone asthma reviews (n = 64) in a sample of general practices participating in the IMP2ART trial (implementation n = 4; control n = 6). Analytical methods included: ALFA Toolkit Multi-Channel Video Observation (to code and quantify tasks undertaken); the Patient-Centred Observation Form; and The Behaviour Change Counselling Index (to assess patient-centeredness and behaviour change counselling used by HCPs).
Results
HCPs mostly spent time during routine asthma reviews discussing: an individual's asthma condition and management (average of 27.8% of consultation time); collaboratively reviewing and completing a personalised asthma action plan (6.3%) and training for practical self-management activities (5.4%). Areas of patient-centred care delivery and behavioural discussions included: creating and maintaining relationships, discussing asthma action plans and medication reconciliation. Professionals in IMP2ART implementation group practices delivered more SSM strategies. Comparison of face-to-face and remote consultations found no significant differences in HCP delivery of SSM.
Conclusions
HCPs in UK primary care spent half the time in both face-to-face and remote asthma reviews delivering components of SSM suggesting that either mode of delivery may be acceptable. Reviews carried out in IMP2ART implementation group practices demonstrated more behaviour change and collaborative SSM strategies compared to those in the control group.
Patient and Public Contribution
Asthma UK Centre for Applied Research (AUKCAR) PPI members were involved throughout, including project conception, providing feedback on participant-facing documents, and discussing implications of study findings.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


