Lessons learned from implementing laparoscopic common bile duct exploration at a safety net hospital
IF 3.2
2区 医学
Q1 SURGERY
引用次数: 0
Abstract
Background
Mounting evidence favors one-stage laparoscopic cholecystectomy with common bile duct exploration over endoscopic retrograde cholangiopancreatography with cholecystectomy for choledocholithiasis. However, laparoscopic cholecystectomy with common bile duct exploration remains underused. In 2020, our center initiated a laparoscopic cholecystectomy with common bile duct exploration program for choledocholithiasis. This study compares the experience and outcomes of laparoscopic cholecystectomy with common bile duct exploration compared with endoscopic retrograde cholangiopancreatography with cholecystectomy at a safety net hospital.
Methods
This single-center, retrospective study analyzed data from 179 patients admitted with choledocholithiasis from 2019 to 2023. Demographics, preoperative investigations, intraoperative details, and postoperative outcomes were evaluated.
Results
The study included 179 patients (55.6 ± 21.0 years, 66% female) with American Society of Anesthesiologists Physical Status Classification System score III (II–III) and body mass index 29 kg/m2 (25.8–35.5 kg/m2). Of these, 148 underwent endoscopic retrograde cholangiopancreatography with cholecystectomy and 31 underwent laparoscopic cholecystectomy with common bile duct exploration. Demographic and preoperative data were similar between groups. Laparoscopic cholecystectomy with common bile duct exploration achieved a 74.2% success rate. Laparoscopic cholecystectomy with common bile duct exploration’s average operative time was 180 (139–213) minutes, with a 3.2% postoperative bile leak and 35.4% requiring postoperative ERCP. Median lengths of stay were 3 (1–4) for laparoscopic cholecystectomy with common bile duct exploration and 4 days (3–7) for endoscopic retrograde cholangiopancreatography with cholecystectomy (Z = –3.16, P = .002). The number of readmissions were 1.2 ± 0.4 for laparoscopic cholecystectomy with common bile duct exploration and 1.9 ± 1.3 for endoscopic retrograde cholangiopancreatography with cholecystectomy (t = 1.43, P = .08). Additional procedures for choledocholithiasis were performed in 36% of laparoscopic cholecystectomy with common bile duct exploration and 79% of ERCP + LC cases (χ2 = 21.7, P < .0001).
Conclusion
The study highlights challenges in implementing laparoscopic cholecystectomy with common bile duct exploration at a safety net hospital. Results support laparoscopic cholecystectomy with common bile duct exploration over endoscopic retrograde cholangiopancreatography, with cholecystectomy, with shorter stays, fewer readmissions, and fewer additional procedures reported. Laparoscopic cholecystectomy with common bile duct exploration remains underused, with only 17.3% of patients who underwent one-stage laparoscopic cholecystectomy with common bile duct exploration. Further research is needed for laparoscopic cholecystectomy with common bile duct exploration’s expansion as the superior choledocholithiasis treatment.
一家安全网医院实施腹腔镜胆总管探查术的经验教训。
背景:越来越多的证据表明,与内镜逆行胰胆管造影胆囊切除术治疗胆总管结石相比,一步式腹腔镜胆囊切除术联合胆总管探查术更受青睐。然而,带总胆管探查的腹腔镜胆囊切除术仍未得到充分利用。2020 年,我们中心启动了腹腔镜胆囊切除术联合胆总管探查治疗胆总管结石的项目。本研究比较了一家安全网医院的腹腔镜胆囊切除术联合胆总管探查术与内镜逆行胰胆管造影联合胆囊切除术的经验和结果:这项单中心回顾性研究分析了2019年至2023年期间收治的179例胆总管结石患者的数据。对人口统计学、术前检查、术中细节和术后结果进行了评估:研究共纳入 179 名患者(55.6±21.0 岁,66% 为女性),美国麻醉医师协会体格状态分类系统评分 III(II-III),体重指数 29 kg/m2(25.8-35.5 kg/m2)。其中,148 人接受了内镜逆行胰胆管造影术和胆囊切除术,31 人接受了腹腔镜胆囊切除术和胆总管探查术。两组患者的人口统计学和术前数据相似。腹腔镜胆囊切除术联合胆总管探查术的成功率为74.2%。腹腔镜胆囊切除术联合胆总管探查术的平均手术时间为 180 (139-213) 分钟,术后胆漏率为 3.2%,35.4% 的患者术后需要进行 ERCP。腹腔镜胆囊切除术联合胆总管探查术的中位住院时间为 3 天(1-4 天),内镜逆行胰胆管造影联合胆囊切除术的中位住院时间为 4 天(3-7 天)(Z = -3.16,P = .002)。腹腔镜胆囊切除术合并胆总管探查术的再入院次数为 1.2 ± 0.4,内镜逆行胰胆管造影术合并胆囊切除术的再入院次数为 1.9 ± 1.3(t = 1.43,P = .08)。36%的腹腔镜胆囊切除术合并胆总管探查和79%的ERCP+LC病例因胆总管结石进行了额外手术(χ2 = 21.7,P < .0001):本研究强调了在一家安全网医院实施腹腔镜胆囊切除术加总胆管探查所面临的挑战。研究结果表明,腹腔镜胆囊切除术联合胆总管探查术比内镜逆行胰胆管造影术联合胆囊切除术的住院时间更短、再入院率更低、报告的额外手术更少。带有胆总管探查的腹腔镜胆囊切除术仍未得到充分利用,只有 17.3% 的患者接受了带有胆总管探查的单阶段腹腔镜胆囊切除术。腹腔镜胆囊切除术联合胆总管探查作为胆总管结石的最佳治疗方法还需进一步研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
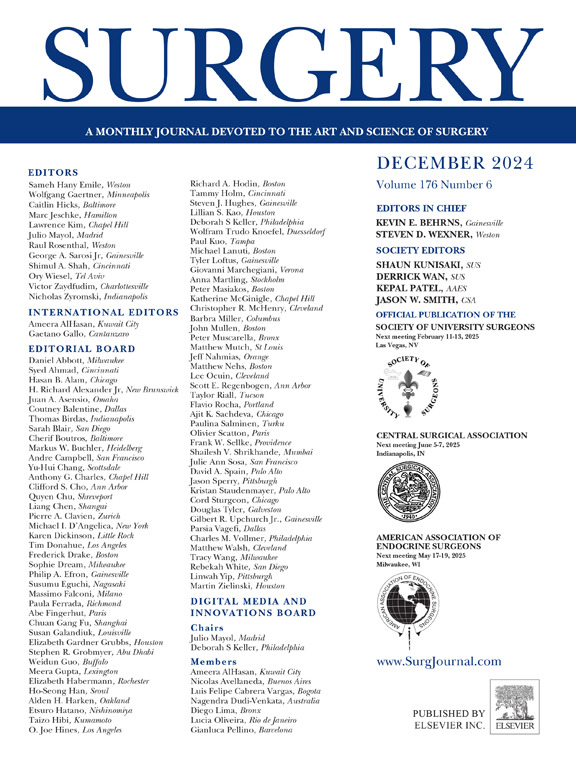
Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


