Non-early catheter ablation vs drug therapy in atrial fibrillation: Results from the CABANA trial
IF 5.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
Early rhythm control reduces the risk of cardiovascular events in patients with atrial fibrillation (AF). Despite the superiority of catheter ablation in maintaining sinus rhythm, the knowledge gaps regarding the prognostic benefits of non-early (onset of AF ≥1 year) ablation remain.
Objective
The study aimed to describe outcomes of non-early AF in the CABANA trial.
Methods
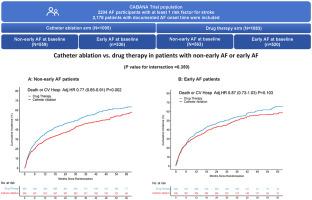
CABANA randomized AF participants to catheter ablation or drug therapy. The primary end point was a composite of death, disabling stroke, serious bleeding, or cardiac arrest. Secondary end points included all-cause mortality and all-cause mortality or cardiovascular hospitalization.
Results
A total of 2178 patients (median age, 67 years; 810 [37.2%] female) were included, 1122 (51.5%) with non-early AF. For the primary outcome, the adjusted hazard ratio (aHR) of ablation vs drug therapy was 0.83 (95% confidence interval [CI], 0.53–1.30; P = .413) in non-early AF patients and 0.78 (95% CI, 0.52–1.16; P = .220) in early AF patients (interaction P value = .787). Non-early ablation resulted in a relative reduction of 26% and 23% in all-cause mortality (aHR, 0.74; 95% CI, 0.42–1.33; P = .314) and all-cause mortality or cardiovascular hospitalization (aHR, 0.77; 95% CI, 0.65–0.91; P = .002), respectively. After exclusion of patients with prior heart failure, non-early AF patients receiving ablation still had a significantly lower risk of all-cause mortality or cardiovascular hospitalization (aHR, 0.78; 95% CI, 0.65–0.93; P = .005).
Conclusion
Non-early AF patients may benefit from catheter ablation similar to early AF patients. Catheter ablation may be an effective treatment strategy to reduce the composite risk of all-cause mortality or cardiovascular hospitalization in non-early AF patients.
心房颤动的非早期导管消融与药物治疗:CABANA 试验结果。
背景:尽早控制心律可降低心房颤动(房颤)患者发生心血管事件的风险。尽管导管消融在维持窦性心律方面具有优越性,但关于非早期(心房颤动发病≥1年)消融的预后益处仍存在知识空白:描述 CABANA 试验中非早期房颤的疗效:CABANA 试验将房颤参与者随机分为导管消融和药物治疗两种。主要终点是死亡、致残性中风、严重出血或心脏骤停的综合结果。次要终点包括全因死亡率、全因死亡率或心血管住院率:共纳入 2178 名患者(中位年龄 67 岁;810 名[37.2%]女性),其中 1122 名(51.5%)为非早期房颤患者。就主要结果而言,消融与药物治疗的调整危险比(aHR)在非早期房颤患者中为 0.83(95% CI 0.53-1.30,P=0.413),在早期房颤患者中为 0.78(95% CI 0.52-1.16,P=0.220)(交互 P 值 =0.787)。非早期消融使全因死亡率(aHR 0.74,95% CI 0.42-1.33,P=0.314)和全因死亡率或心血管住院率(aHR 0.77,95% CI 0.65-0.91,P=0.002)分别相对降低了 26% 和 23%。排除既往有心力衰竭的患者后,接受消融治疗的非早期房颤患者的全因死亡或心血管住院风险仍显著降低(aHR 0.78,95% CI 0.65-0.93,P=0.005):结论:非早期房颤患者与早期房颤患者一样,可从导管消融术中获益。无论是否有心衰病史,导管消融都可能是降低非早期房颤患者全因死亡或心血管住院综合风险的有效治疗策略。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Heart rhythm
医学-心血管系统
CiteScore
10.50
自引率
5.50%
发文量
1465
审稿时长
24 days
期刊介绍:
HeartRhythm, the official Journal of the Heart Rhythm Society and the Cardiac Electrophysiology Society, is a unique journal for fundamental discovery and clinical applicability.
HeartRhythm integrates the entire cardiac electrophysiology (EP) community from basic and clinical academic researchers, private practitioners, engineers, allied professionals, industry, and trainees, all of whom are vital and interdependent members of our EP community.
The Heart Rhythm Society is the international leader in science, education, and advocacy for cardiac arrhythmia professionals and patients, and the primary information resource on heart rhythm disorders. Its mission is to improve the care of patients by promoting research, education, and optimal health care policies and standards.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


