SIADH secondary to rhino-orbito-cerebral mucormycosis: A case report
Abstract
Key Clinical Message
Invasive fungal mucormycosis and its outcome as SIADH and orbital apex syndrome is uncommon. Mucormycosis in paranasal sinuses can even lead to intracranial invasion and its treatment with the use of amphotericin B can cure improve the prognosis of the disease. Early diagnosis and prompt treatment with antifungal, endoscopic surgery, and controlling of diabetes can be beneficial.
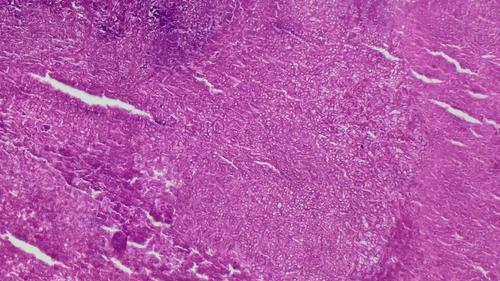
Mucormycosis is an opportunistic invasive fungal infection which is rare and fatal and can even cause intracranial invasion leading to SIADH. The infrequency with which mucormycosis with SIADH is encountered makes it a formidable diagnostic challenge. 70-year-old women uncontrolled diabetes mellitus presented with bilious vomiting and persistent headache with ptosis, proptosis, absence of extraocular movement, pupillary light reflex, and light perception of left eye. Radiographic investigation, KOH mount, and Biopsy showed mucormycosis in sinus with intracranial extension leading to SIADH. Further investigation revealed hyponatremia, decreased plasma osmolality. Then, when diabetes was controlled and hydrocortisone and amphotericin was given along with Endoscopic sinus debridement, SIADH was well controlled. This case illustrates the potential of mucormycosis in paranasal sinuses can even lead to intracranial invasion and its treatment with the use of amphotericin B can cure improve the prognosis of the disease. Prompt diagnosis through clinical history, radiological investigation, and laboratory parameters are important and its treatment is crucial for the better prognosis.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


