Burden of liver steatosis and liver fibrosis in a large cohort of people living with HIV
Abstract
Background
Liver steatosis (LS) and liver fibrosis (LF) can increase the risk of cardiovascular disease in people with HIV, but their prevalence and associated factors are poorly understood. This study aimed to assess the prevalence of and factors associated with LS and LF in a large cohort of people with HIV.
Methods
We conducted a cross-sectional study of consecutive people with HIV attending the Clinic of Barcelona from September 2022 to September 2023, excluding those with chronic B or/and C hepatitis virus coinfection. LS was assessed using the Hepatic Steatosis Index (HSI) and Fatty Liver Index (FLI), and LF was assessed using the Non-Alcoholic Fatty Liver Disease Fibrosis Score (NFS), Fibrosis-4 score (FIB-4), and the European AIDS Clinical Society (EACS) algorithm in both the whole cohort (cohort 1) and in a specific cohort more susceptible to liver disease (cohort 2). We identified independent variables associated with LS and LF using logistic regression.
Results
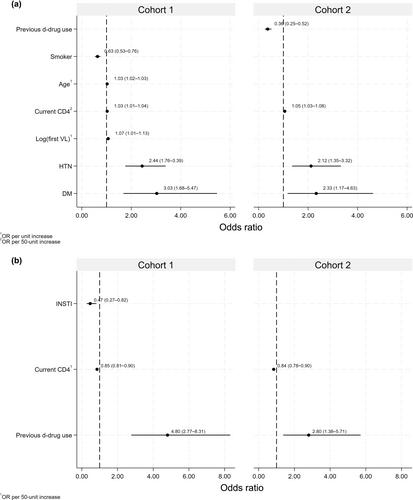
Cohort 1 included 4664 people with HIV; 76% and 37% of them had available HSI and FLI data, LS was present in 28% and 19%, respectively. LF risk was present in 1%, 2%, and 1% of people with HIV according to NFS, FIB-4, and EACS algorithm scores, respectively. Cohort 2 included 1345 people with HIV; 60% and 30% of them had available HSI and FLI data, LS affected 55% and 43% and LF 2%, 5%, or 3%, respectively. Factors associated with LS included current CD4 cell count, diabetes, and hypertension, whereas LF was associated with previous exposure to dideoxynucleoside drugs and current CD4 to LF. Current integrase strand transfer inhibitor (INSTI) therapy appeared protective for LF in cohort 1.
Conclusions
In this study, one in four people with HIV had LS, and the prevalence rose to one in two in those with cardiovascular risk factors. The prevalence of LF was low, but it should be considered in older people with HIV with low CD4 counts or high aspartate transaminase levels. A possible protective effect from INSTIs deserves further investigation.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


