The Optimal Radiotherapy Strategy for Patients With Small Cell Lung Cancer and Brain Metastasis: A Retrospective Analysis
Abstract
Background
Extensive-stage small cell lung cancer (ES-SCLC) is a notoriously aggressive malignancy frequently associated with brain metastases (BMs), presenting substantial therapeutic challenges. This study delves into the effectiveness of immunotherapy combined with diverse radiotherapy, especially the influence of brain radiotherapy (BRT) on survival outcomes in the immunotherapy era.
Methods
ES-SCLC patients treated at Xiangya Hospital and Xiangya Boai Hospital from February 2020 to June 2024 were retrospectively included. The study focused on patients receiving immune checkpoint inhibitors (ICIs). Metrics included overall survival (OS) and progression-free survival (PFS), employing univariate and multivariate Cox regression models for statistical analysis.
Results
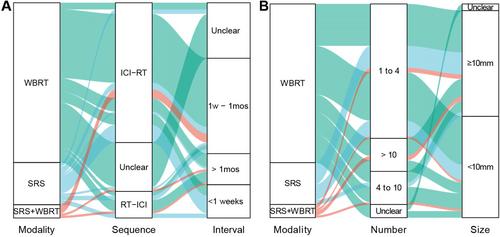
A total of 393 patients with ES-SCLC who received ICIs were included in the study. Within the entire cohort, the presence of baseline BMs did not statistically affect OS or PFS. However, thoracic radiotherapy (TRT) was identified as a favorable prognostic factor for both OS and PFS. BRT demonstrated a beneficial effect on OS across both the general cohort and the baseline_BMs subgroup. In patients from the baseline_BMs subgroup who had previously undergone TRT, ICIs plus BRT did not significantly improve OS compared to ICIs alone. Conversely, for patients who had not received prior TRT, adding BRT to ICIs significantly enhanced OS. Among the patients who underwent BRT, 71 received whole brain radiotherapy (WBRT) while 19 opted for stereotactic radiosurgery (SRS). No significant differences in OS and PFS were observed between the SRS and WBRT modalities. The sequence of ICIs relative to BRT was found to influence PFS adversely. Administering BRT before ICIs (RT-ICI) was associated with worse PFS compared to administering ICIs followed by BRT (ICI-RT). Additionally, no significant differences in OS and PFS were noted among the three subgroups defined by varying intervals between ICIs and BRT. For patients without baseline BMs, TRT and prophylactic cranial irradiation were associated with delayed onset of brain metastases.
Conclusions
Our study underscores the importance of optimizing treatment strategies and considering the timing and integration of radiotherapy and immunotherapy to improve outcomes for patients with ES-SCLC, particularly those at risk of or presenting with BMs.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


