Transarterial Infusion Chemotherapy and Embolization for Patients With Unresectable Advanced Cancer of Stomach or Gastroesophageal Junction: A Retrospective Study
Abstract
Purpose
The feasibility of transarterial infusion chemotherapy and embolization (TAICE) in the treatment of advanced gastric cancer remains unclear. This study explored the value of TAICE in patients with unresectable locally advanced or metastatic cancer of stomach or gastroesophageal junction (GEJ).
Methods
Patients with unresectable gastric cancer who received TAICE for tumor hemorrhage cessation were enrolled in this retrospective study. TAICE was performed using the Seldinger method. The tumor feeding artery was selected for infusion chemotherapy and then was embolized by microspheres or gelatin sponge. Patients involved in this study received one to four cycles TAICE with one to three drugs in the regimen. The possibility of surgery was evaluated after TAICE. Objective response rate (ORR), disease control rate (DCR), R0 resection rate, pathological complete remission (pCR) rate, major pathological remission (MPR) rate, progression-free survival (PFS), overall survival (OS), and safety were analyzed.
Results
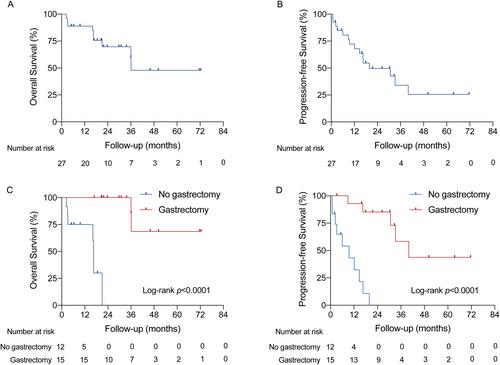
Between January 2015 and December 2020, a total of 27 patients received a median of 2 (range, 1–4) cycles of TAICE. ORR and DCR were 33.3% and 74.0%, respectively. Eighteen patients received surgery, and 15 of them underwent gastrectomy and D2 lymph node dissection, with an R0 resection rate of 83.3% (15/18). Four (26.7%, 4/15) patients achieved MPR, but none achieved pCR. The median PFS was 19.8 months (95%CI, 12.1–40.0), and the median OS was 36.1 months (95%CI, 21.0–not reached). Patients with gastrectomy had significantly longer PFS (40.0 vs. 9.5 months, p < 0.0001) and OS (not reached vs. 16.6 months, p < 0.0001) than those without gastrectomy. All the TAICE-related adverse events were manageable, with the most common being fatigue (100%), nausea (63.0%), and vomiting (55.6%). No severe surgical complications occurred.
Conclusion
TAICE was well-tolerated and could be a potential therapy to provide opportunity of surgery for patients with unresectable advanced gastric or GEJ cancer.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


