Mini nutritional assessment short form as a predictor of mortality among older adults with dementia residing in group homes: A 5-year longitudinal study
IF 2.9
Q3 NUTRITION & DIETETICS
引用次数: 0
Abstract
Background & aims
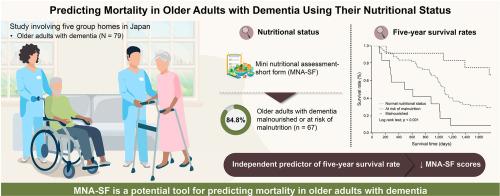
Many people with dementia frequently experience various health-related problems and are known to have poor nutritional status. However, very few studies have examined the nutritional status of dementia residents in group homes, which play an important role in a society-wide system of support for people with dementia, or the relationship between nutritional status and long-term prognosis. This study was conducted to determine the nutritional status of group-home residents and to examine the relationship between nutritional status and the 5-year survival rate.
Methods
Participant characteristic (e.g., age, sex, body mass index, and medical history) and Mini Nutritional Assessment-Short Form (MNA-SF), Barthel index (BI), and Clinical Dementia Rating (CDR) data were collected from 79 older people (12 men/67 women; mean age: 88.3 ± 5.5 years) residing in 5 group homes as a baseline survey. Mortality data were obtained from medical records using an endline survey.
Results
The nutritional status of the participants using the MNA-SF was normal, at risk of malnutrition, and malnourished in 15.2 % (n = 12), 69.6 % (n = 55), and 15.2 % (n = 12) of participants, respectively. Following the survey, mortality data were collected for 5 years, and the 5-year survival rates were 64.3 % in those with normal nutritional status, 30.4 % in those at risk of malnutrition, and 9.1 % in the malnourished group, with a significant difference observed in the Kaplan–Meier analysis (p < 0.001). The hazard ratio for the MNA-SF scores and survival rates adjusted for sex, age, BI, and CDR were significant 0.80 [0.69–0.93, p = 0.003].
Conclusion
This study showed that 84.8 % of patients with dementia residing in group homes were malnourished or at risk of malnutrition and that low MNA-SF levels were an independent determinant of the 5-year survival rate.
迷你营养评估简表可预测住在集体之家的老年痴呆症患者的死亡率:一项为期 5 年的纵向研究。
背景与目的:众所周知,许多痴呆症患者经常会遇到各种与健康相关的问题,而且营养状况较差。然而,很少有研究对在全社会痴呆症患者支持系统中扮演重要角色的集体之家的痴呆症患者的营养状况或营养状况与长期预后之间的关系进行调查。本研究旨在确定集体之家居民的营养状况,并探讨营养状况与5年存活率之间的关系:作为基线调查,收集了居住在 5 家集体之家的 79 名老年人(12 名男性/67 名女性;平均年龄:88.3 ± 5.5 岁)的特征(如年龄、性别、体重指数和病史)、迷你营养评估简表(MNA-SF)、巴特尔指数(BI)和临床痴呆评级(CDR)数据。通过终点调查从医疗记录中获得了死亡率数据:使用 MNA-SF 测量参与者的营养状况,正常、有营养不良风险和营养不良的参与者分别占 15.2%(n = 12)、69.6%(n = 55)和 15.2%(n = 12)。调查结束后,收集了 5 年的死亡率数据,营养状况正常者的 5 年存活率为 64.3%,有营养不良风险者为 30.4%,营养不良组为 9.1%,卡普兰-梅耶尔分析中观察到了显著差异(P < 0.001)。经性别、年龄、BI 和 CDR 调整后,MNA-SF 评分和生存率的危险比为 0.80 [0.69-0.93,p = 0.003],差异显著:这项研究表明,84.8%居住在集体之家的痴呆症患者存在营养不良或营养不良风险,而低MNA-SF水平是5年生存率的独立决定因素。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Clinical nutrition ESPEN
NUTRITION & DIETETICS-
CiteScore
4.90
自引率
3.30%
发文量
512
期刊介绍:
Clinical Nutrition ESPEN is an electronic-only journal and is an official publication of the European Society for Clinical Nutrition and Metabolism (ESPEN). Nutrition and nutritional care have gained wide clinical and scientific interest during the past decades. The increasing knowledge of metabolic disturbances and nutritional assessment in chronic and acute diseases has stimulated rapid advances in design, development and clinical application of nutritional support. The aims of ESPEN are to encourage the rapid diffusion of knowledge and its application in the field of clinical nutrition and metabolism. Published bimonthly, Clinical Nutrition ESPEN focuses on publishing articles on the relationship between nutrition and disease in the setting of basic science and clinical practice. Clinical Nutrition ESPEN is available to all members of ESPEN and to all subscribers of Clinical Nutrition.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


