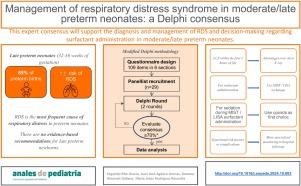
Management of respiratory distress syndrome in moderate/late preterm neonates: A Delphi consensus
引用次数: 0
Abstract
Introduction
Respiratory distress syndrome (RDS) is the most frequent cause of respiratory distress in preterm neonates. In the management of RDS, surfactant plays a pivotal role, but there are no evidence-based recommendations for moderate/late preterm neonates (32–36 weeks).
Methods
A scientific committee developed a questionnaire with 53 questions addressing diagnosis, treatment, potential complications and future trends in RDS specifically focused on moderate and late preterm neonates. This was followed by the performance of a Delphi survey of expert neonatologists.
Results
Consensus was reached on 98 of the 109 items. The recommendations for the diagnosis of RDS included performing a lung ultrasound and including mild respiratory distress, transient tachypnoea of the newborn, congenital pneumonia and primary pulmonary hypertension in the differential diagnosis. Most panellists agreed on the need for studies that determine the benefit/harm balance, clinical profile and methods of surfactant administration in moderate/late preterm neonates. All respondents would use the MIST approach with devices specifically designed for surfactant administration. Regarding sedation measures during MIST, most participants agreed on the use of nonpharmacological interventions and, if these proved ineffective, an opioid. All respondents agreed that moderate/late preterm neonates are at increased risk of neonatal morbidity and mortality, particularly respiratory problems, and considered the need for more specialised monitoring in hospital follow-up visits in neonates with associated risk factors or a history of complications in the neonatal period. Finally, all respondents agreed that there is a lack of studies identifying risk factors and medium-term adverse outcomes in moderate/late preterm neonates.
Conclusion
This expert consensus will help with the diagnosis and management of RDS and guide decision-making about surfactant administration in moderate/late preterm neonates.
中度/晚期早产新生儿呼吸窘迫综合征的管理:德尔菲共识。
简介呼吸窘迫综合征(RDS)是早产新生儿呼吸窘迫的最常见原因。在 RDS 的治疗中,表面活性物质起着关键作用,但目前还没有针对中度/晚期早产新生儿(32-36 周)的循证建议:方法:一个科学委员会编制了一份调查问卷,其中包含 53 个问题,涉及 RDS 的诊断、治疗、潜在并发症和未来趋势,特别关注中度和晚期早产新生儿。随后对新生儿专家进行了德尔菲调查:结果:在 109 个项目中,有 98 个项目达成了共识。诊断 RDS 的建议包括进行肺部超声波检查,并将轻度呼吸困难、新生儿一过性呼吸困难、先天性肺炎和原发性肺动脉高压纳入鉴别诊断。大多数小组成员一致认为有必要开展研究,以确定中度/晚期早产新生儿表面活性物质给药的利弊平衡、临床概况和方法。所有受访者都表示将使用 MIST 方法和专门为表面活性物质给药设计的设备。关于 MIST 期间的镇静措施,大多数参与者都同意使用非药物干预措施,如果无效,则使用阿片类药物。所有答复者都认为,中度/晚期早产新生儿的新生儿发病率和死亡率,尤其是呼吸系统问题的风险会增加,并认为有必要在医院随访时对有相关风险因素或新生儿期并发症病史的新生儿进行更专业的监测。最后,所有受访者一致认为,目前缺乏对中度/晚期早产新生儿风险因素和中期不良后果的研究:该专家共识将有助于 RDS 的诊断和管理,并为中晚期早产新生儿使用表面活性物质的决策提供指导。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


