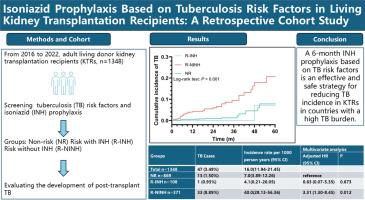
Isoniazid prophylaxis based on tuberculosis risk factors in living kidney transplantation recipients: A retrospective cohort study
IF 4.9
2区 医学
Q1 INFECTIOUS DISEASES
International Journal of Antimicrobial Agents
Pub Date : 2024-10-31
DOI:10.1016/j.ijantimicag.2024.107375
引用次数: 0
Abstract
Background
Tuberculosis (TB) is a major and severe opportunistic infection among solid organ transplant recipients. Chemoprophylaxis is advised for those with latent tuberculosis infection. However, the effectiveness of an isoniazid (INH) prophylactic approach based on TB risk factors remains uncertain.
Methods
This study included all living-donor kidney transplant recipients between January 2016 and December 2022. The recipients were categorized into three groups: the risk group with INH (R-INH), the risk group without INH (R-NINH), and the non-risk group (NR), based on the presence of TB risk factors and INH usage. The R-INH group received a 6-month INH prophylactic regimen to prevent post-transplant TB infection. The incidence of active TB among the groups was assessed.
Results
A total of 1348 patients were divided into R-INH (n = 108), R-NINH (n = 371), and NR (n = 869). Forty-seven patients (3.49%) developed TB with an incidence rate of 16.0 per 1000 person-years. Compared to NR, the TB incidence in R-INH was not statistically different (hazard ratios, 0.55, 95% confidence interval, 0.07–4.21, P = 0.564), whereas it was significantly higher in R-NINH (hazard ratios, 5.04, 95% confidence interval, 2.64–9.62, P < 0.001). The median time from transplantation to TB was 19 months (interquartile range: 6–39), and 18 patients (38.3%) were diagnosed within 1 year of transplantation. Ninety-four patients (87.0%) completed INH prophylaxis, with adverse events including two cases of hepatotoxicity (1.85%) and one case of peripheral neuritis (0.93%).
Conclusions
A 6-month INH regimen based on TB risk factors is effective and well-tolerated for preventing post-transplant TB in kidney transplant recipients.
基于活体肾移植受者结核病风险因素的异烟肼预防:一项回顾性队列研究
背景:结核病(TB)是实体器官移植受者中主要的严重机会性感染。建议潜伏肺结核感染者(LTBI)进行化学预防。然而,基于结核病风险因素的异烟肼(INH)预防方法的有效性仍不确定:本研究纳入了 2016 年 1 月至 2022 年 12 月期间的所有活体供肾移植受者(KTR)。根据是否存在结核病风险因素和 INH 使用情况,将受者分为三组:使用异烟肼的风险组(R-INH)、不使用异烟肼的风险组(R-NINH)和非风险组(NR)。R-INH 组接受为期 6 个月的 INH 预防治疗,以预防移植后结核病感染。对各组间活动性肺结核的发病率进行了评估:共有 1348 名患者被分为 R-INH 组(108 人)、R-NINH 组(371 人)和 NR 组(869 人)。47名患者(3.49%)患上了肺结核,发病率为每千人年16.0例。与 NR 相比,R-INH 的肺结核发病率没有统计学差异(HR,0.55,95% CI,0.07-4.21,P = 0.564),而 R-NINH 的发病率明显更高(HR,5.04,95% CI,2.64-9.62,P <0.001)。从移植到肺结核的中位时间为 19 个月(IQR:6-39),18 名患者(38.3%)在移植后一年内确诊。94名患者(87.0%)完成了INH预防治疗,不良反应包括2例肝脏毒性(1.85%)和1例周围神经炎(0.93%):结论:根据结核病风险因素制定的为期 6 个月的 INH 方案对预防 KTR 移植后结核病有效且耐受性良好。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
CiteScore
21.60
自引率
0.90%
发文量
176
审稿时长
36 days
期刊介绍:
The International Journal of Antimicrobial Agents is a peer-reviewed publication offering comprehensive and current reference information on the physical, pharmacological, in vitro, and clinical properties of individual antimicrobial agents, covering antiviral, antiparasitic, antibacterial, and antifungal agents. The journal not only communicates new trends and developments through authoritative review articles but also addresses the critical issue of antimicrobial resistance, both in hospital and community settings. Published content includes solicited reviews by leading experts and high-quality original research papers in the specified fields.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


