Clinical significance of intraductal papillary mucinous neoplasms incidentally detected in patients with extrapancreatic gastrointestinal malignancies with a focus on pancreatic cancer development
IF 2.7
2区 医学
Q1 SURGERY
引用次数: 0
Abstract
Background
Intraductal papillary mucinous neoplasm is occasionally detected in the preoperative images of patients with gastrointestinal malignancies. Despite numerous studies examining the incidence of extrapancreatic malignancies in patients with intraductal papillary mucinous neoplasm, limited data exist on the prevalence of intraductal papillary mucinous neoplasm in those with gastrointestinal malignancies. Given that intraductal papillary mucinous neoplasm is a known risk factor for pancreatic cancer, this study aimed to evaluate the prevalence of intraductal papillary mucinous neoplasm in patients who underwent radical surgery for extrapancreatic gastrointestinal malignancies and its impact on pancreatic cancer development.
Methods
We retrospectively reviewed the preoperative computed tomography images of patients who underwent radical surgery for gastrointestinal malignancies between January 2017 and December 2021 for the presence of intraductal papillary mucinous neoplasm. Patients were divided into intraductal papillary mucinous neoplasm and non–intraductal papillary mucinous neoplasm groups, and clinicopathologic features and long-term outcomes, including pancreatic cancer development, were compared between groups.
Results
A total of 814 patients who underwent radical surgery for extrapancreatic gastrointestinal malignancies were included. Among them, 81 patients (10.0%) had intraductal papillary mucinous neoplasm. The median observation period was 39 (0–79) months. Notably, pancreatic cancer developed in 5 patients with intraductal papillary mucinous neoplasm and 1 without. The 5-year cumulative incidences of pancreatic cancer were 8.8% and 0.2% in the intraductal papillary mucinous neoplasm and non–intraductal papillary mucinous neoplasm groups, respectively (P < .001).
Conclusion
Intraductal papillary mucinous neoplasm is frequently detected in the preoperative images of patients with gastrointestinal malignancies and is associated with a significantly higher risk of developing pancreatic cancer. Consequently, long-term surveillance for pancreatic cancer is crucial in patients with intraductal papillary mucinous neoplasm, particularly those with extrapancreatic gastrointestinal malignancies.
在胰腺外消化道恶性肿瘤患者中偶然发现的导管内乳头状黏液瘤的临床意义,重点关注胰腺癌的发展。
背景:导管内乳头状黏液瘤偶尔会在胃肠道恶性肿瘤患者的术前影像中被发现。尽管有许多研究探讨了导管内乳头状粘液瘤患者胰腺外恶性肿瘤的发病率,但有关胃肠道恶性肿瘤患者导管内乳头状粘液瘤发病率的数据却很有限。鉴于导管内乳头状粘液瘤是胰腺癌的一个已知风险因素,本研究旨在评估导管内乳头状粘液瘤在因胰腺外胃肠道恶性肿瘤接受根治性手术的患者中的发病率及其对胰腺癌发展的影响:我们回顾性地查看了2017年1月至2021年12月期间接受胃肠道恶性肿瘤根治术患者的术前计算机断层扫描图像,以确定是否存在导管内乳头状黏液瘤。将患者分为导管内乳头状黏液瘤组和非导管内乳头状黏液瘤组,比较两组患者的临床病理特征和远期预后,包括胰腺癌的发展情况:共纳入了814例因胰腺外消化道恶性肿瘤接受根治手术的患者。其中,81 名患者(10.0%)患有导管内乳头状黏液瘤。中位观察期为 39(0-79)个月。值得注意的是,5 名导管内乳头状粘液瘤患者和 1 名非导管内乳头状粘液瘤患者发生了胰腺癌。导管内乳头状粘液瘤组和非导管内乳头状粘液瘤组的胰腺癌5年累积发病率分别为8.8%和0.2%(P 结论:导管内乳头状粘液瘤组和非导管内乳头状粘液瘤组的胰腺癌5年累积发病率分别为8.8%和0.2%:导管内乳头状粘液瘤经常在胃肠道恶性肿瘤患者的术前影像中被发现,并且与胰腺癌的高风险显著相关。因此,对于导管内乳头状粘液瘤患者,尤其是胰腺外胃肠道恶性肿瘤患者,长期监测胰腺癌至关重要。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
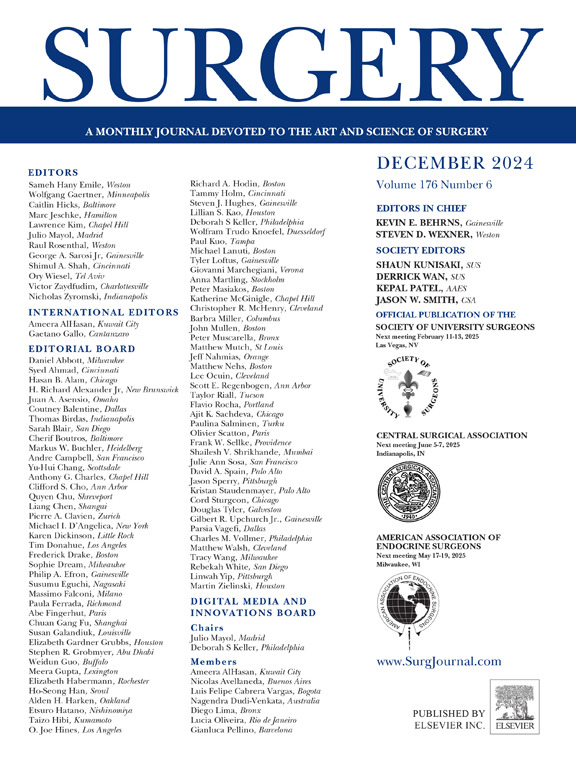
Surgery
医学-外科
CiteScore
5.40
自引率
5.30%
发文量
687
审稿时长
64 days
期刊介绍:
For 66 years, Surgery has published practical, authoritative information about procedures, clinical advances, and major trends shaping general surgery. Each issue features original scientific contributions and clinical reports. Peer-reviewed articles cover topics in oncology, trauma, gastrointestinal, vascular, and transplantation surgery. The journal also publishes papers from the meetings of its sponsoring societies, the Society of University Surgeons, the Central Surgical Association, and the American Association of Endocrine Surgeons.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


