Predicting mid- and late-life dementia risk in primary care: A prognostic study from a national health screening cohort
IF 4.2
2区 医学
Q1 PSYCHIATRY
引用次数: 0
Abstract
The objective of this study is to develop and validate dementia risk prediction models for mid- and late-life individuals that are based on accessible variables within a primary care setting. Using the Korean National Health Insurance Service database (2010–2019), we analyzed 6,696,073 individuals aged 40 and older who participated in a national health screening program over a mean follow-up of 8.95 years. Potential predictors were selected based on a literature review and the available data. Dementia cases were identified using claim-based codes and validated by corresponding prescription information. 5-year dementia risk prediction models for mid-life (40–59 years), and late-life (60+ years) stages were developed using the Cox proportional hazards model. Model performance was assessed through discrimination and calibration. Both models included age, sex, body mass index, smoking, alcohol consumption, physical activity, diabetes, hypertension, dyslipidemia, and chronic kidney disease. The models’ AUROCs were 0.764 for mid-life and 0.743 for late-life. The impact of predictors on dementia risk was consistently stronger in mid-life than in late-life stages. Our models showed good calibration with low-risk estimates in mid-life and overall in late-life. These findings underscore the crucial role of managing modifiable risk factors, particularly during mid-life to reduce dementia risk.
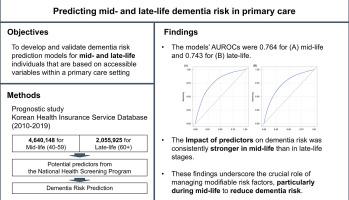
预测初级保健中的中晚期痴呆症风险:一项来自全国健康检查队列的预后研究。
本研究旨在开发和验证基于初级保健环境中可获取变量的中晚年痴呆症风险预测模型。我们利用韩国国民健康保险服务数据库(2010-2019 年)分析了 6,696,073 名 40 岁及以上的人,他们参加了一项全国健康筛查计划,平均随访时间为 8.95 年。我们根据文献综述和现有数据选择了潜在的预测因素。痴呆症病例通过索赔代码进行识别,并通过相应的处方信息进行验证。使用 Cox 比例危险模型建立了中年(40-59 岁)和晚年(60 岁以上)阶段的 5 年痴呆症风险预测模型。通过判别和校准对模型性能进行了评估。两个模型均包括年龄、性别、体重指数、吸烟、饮酒、体力活动、糖尿病、高血压、血脂异常和慢性肾病。中年期和晚年期模型的AUROC分别为0.764和0.743。预测因素对痴呆症风险的影响在中年阶段始终强于晚年阶段。我们的模型显示出良好的校准性,中年期的低风险估计值和晚年期的总体估计值都很高。这些发现强调了管理可改变的风险因素的重要作用,尤其是在中年时期,以降低痴呆症风险。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Psychiatry Research
医学-精神病学
CiteScore
17.40
自引率
1.80%
发文量
527
审稿时长
57 days
期刊介绍:
Psychiatry Research offers swift publication of comprehensive research reports and reviews within the field of psychiatry.
The scope of the journal encompasses:
Biochemical, physiological, neuroanatomic, genetic, neurocognitive, and psychosocial determinants of psychiatric disorders.
Diagnostic assessments of psychiatric disorders.
Evaluations that pursue hypotheses about the cause or causes of psychiatric diseases.
Evaluations of pharmacologic and non-pharmacologic psychiatric treatments.
Basic neuroscience studies related to animal or neurochemical models for psychiatric disorders.
Methodological advances, such as instrumentation, clinical scales, and assays directly applicable to psychiatric research.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


