Low birth weight associations with cardiac structure and function in adults after arterial switch for transposition of the great arteries
IF 1.2
Q4 CARDIAC & CARDIOVASCULAR SYSTEMS
International journal of cardiology. Congenital heart disease
Pub Date : 2024-10-23
DOI:10.1016/j.ijcchd.2024.100550
引用次数: 0
Abstract
Background and aims
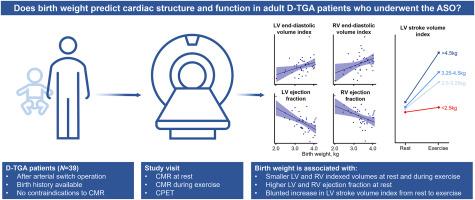
The objective of this study was to assess the associations of birth weight with cardiac structure and function in adults with dextro-transposition of the great arteries (D-TGA) who underwent the arterial switch operation (ASO).
Methods and results
Thirty-nine ASO patients (age 24.4 ± 3.3 years) were included during routine clinical follow-up from July 2019 to December 2021. All patients underwent cardiopulmonary exercise testing and cardiac magnetic resonance imaging at rest and during exercise. Early-life characteristics, including birth weight, were extracted from electronic medical health records. Linear regression analysis showed that lower birth weight was associated with smaller left ventricular (LV) and right ventricular (RV) end-diastolic volume index (LV: −14.5 mL/m2 [95 % confidence interval, CI: −26.5 to −2.5] per 1-kg decrease in birth weight, p = 0.04; RV: −11.2 mL/m2 [-20.7 to −1.7] per 1-kg decrease in birth weight, p = 0.03). Lower birth weight was associated with greater LV and RV ejection fraction at rest (LV: +8.5 % [+4.4 to +12.5] per 1-kg decrease in birth weight, p < 0.001); RV: +8.1 % [+2.8 to +13.4] per 1-kg decrease in birth weight, p = 0.005). Furthermore, lower birth weight was associated with an attenuated increase in LV stroke volume index from rest to peak exercise (−5.2 mL/m2 [-9.3 to −1.2] per 1-kg decrease in birth weight, p = 0.02).
Conclusions
Birth weight may be a novel risk factor for adverse cardiac remodeling in adult ASO patients. Further research is needed to delineate the mechanisms underlying the associations between birth weight and cardiac remodeling ASO patients as well as the broader adult CHD population.
低出生体重与大动脉转位术后成人心脏结构和功能的关系
背景和目的本研究旨在评估接受动脉转换手术(ASO)的成人大动脉右侧横位(D-TGA)患者的出生体重与心脏结构和功能的关系。所有患者均接受了静息和运动时的心肺运动测试和心脏磁共振成像。从电子医疗健康记录中提取了包括出生体重在内的早期生活特征。线性回归分析表明,较低的出生体重与较小的左心室(LV)和右心室(RV)舒张末期容积指数(LV:出生体重每下降 1 公斤,左心室和右心室舒张末期容积指数为-14.5 mL/m2 [95 % 置信区间,CI:-26.5 至-2.5],p = 0.04;右心室舒张末期容积指数为-11.2 mL/m2 [95 % 置信区间,CI:-11.2 至-2.5],p = 0.04:-出生体重每下降 1 公斤,RV:-11.2 mL/m2 [-20.7 至 -1.7],p = 0.03)。出生体重每下降 1 公斤,左心室:+8.1 % [+2.8 至 +13.4],p = 0.005)。此外,出生时体重较低与左心室搏出量指数从静息到运动峰值的增加减弱有关(出生时体重每减少 1 公斤,左心室搏出量指数增加-5.2 mL/m2 [-9.3 至 -1.2] ,p = 0.02)。出生体重可能是导致成年 ASO 患者心脏重塑不良的新风险因素,需要进一步研究来阐明出生体重与 ASO 患者以及更广泛的成年心脏病人群心脏重塑之间的关联机制。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

International journal of cardiology. Congenital heart disease
Cardiology and Cardiovascular Medicine
自引率
0.00%
发文量
0
审稿时长
83 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


