Deciphering the cardioprotective effects of statins in anthracycline-related cardiac dysfunction: A systematic review and meta-analysis
IF 4.3
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
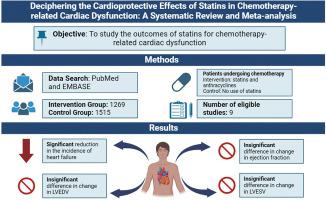
Cancer induced chronic inflammation and cancer drugs effects on the vascular system can lead to rapidly progressing atherosclerotic burden. Statins drugs are known to reduce atherosclerotic plaque burden and inflammation. We studied outcomes of statins for anthracycline-related cardiac dysfunction (ARCD).
Methods
We conducted an online systematic search on PubMed and Embase to identify studies assessing statins' role in alleviating ARCD. We selected 9 studies that had patients with ARCD and use of statins. We primarily focused on outcomes including incidence of heart failure (HF), mean changes in left ventricular ejection fraction (LVEF), end-diastolic volume (LVEDV), and end-systolic volume (LVESV) from baseline. Odds ratios (OR) were calculated using a random effect model in R-statistics.
Results
Among 9 studies with a total of 2784 patients we noticed a significant reduction in the incidence of HF among patients administered statins, with an OR of 0.52 (95 % CI 0.37-0.74, p < 0.0003), indicating a substantial protective effect. However, the mean changes in EF, LVEDV, and LVESV from baseline, represented by Hedges's g of 1.09 (95 % CI -0.40 to 2.57, p = 0.15), 0.91 (95 % CI -1.69 to 3.51, p = 0.47), and 1.32 (95 % CI -2.30 to 4.94, p = 0.49) respectively, were not statistically significant. (Figure 1).
Conclusion
Our meta-analysis confirms statins' effectiveness in reducing risk of ARCD. However, their influence on EF, LVEDV, and LVESV remains uncertain, warranting further study.
解密他汀类药物在蒽环类药物相关心功能障碍中的心脏保护作用:系统回顾和荟萃分析
背景癌症诱发的慢性炎症和抗癌药物对血管系统的影响可导致动脉粥样硬化负担迅速加重。众所周知,他汀类药物可减少动脉粥样硬化斑块的负担和炎症。我们研究了他汀类药物治疗蒽环类相关心功能不全(ARCD)的效果。方法我们在PubMed和Embase上进行了在线系统搜索,以确定评估他汀类药物在缓解ARCD方面作用的研究。我们选择了 9 项有 ARCD 患者并使用他汀类药物的研究。我们主要关注的结果包括心力衰竭(HF)的发生率、左心室射血分数(LVEF)、舒张末期容积(LVEDV)和收缩末期容积(LVESV)与基线相比的平均变化。结果在9项研究共2784名患者中,我们注意到服用他汀类药物的患者心房颤动发病率显著降低,OR值为0.52(95 % CI 0.37-0.74,p <0.0003),这表明他汀类药物具有很强的保护作用。然而,EF、LVEDV 和 LVESV 与基线相比的平均变化分别为 1.09(95 % CI -0.40 至 2.57,p = 0.15)、0.91(95 % CI -1.69 至 3.51,p = 0.47)和 1.32(95 % CI -2.30 至 4.94,p = 0.49),无统计学意义。(我们的荟萃分析证实了他汀类药物在降低 ARCD 风险方面的有效性。然而,他汀类药物对 EF、LVEDV 和 LVESV 的影响仍不确定,值得进一步研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

American journal of preventive cardiology
Cardiology and Cardiovascular Medicine
CiteScore
6.60
自引率
0.00%
发文量
0
审稿时长
76 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


