The interplay between osteoarthritis and osteoporosis: Mechanisms, implications, and treatment considerations – A narrative review
IF 3.9
引用次数: 0
Abstract
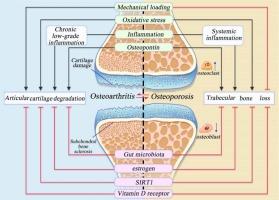
This comprehensive review examines the relationship between osteoarthritis (OA) and osteoporosis (OP), two common disorders in the elderly. OA involves joint cartilage degeneration and pain, while OP leads to fractures due to reduced bone mass. Despite different pathologies, both conditions share risk factors such as age and genetics. Studies reveal mixed results: some show higher bone mineral density (BMD) in OA patients, suggesting an inverse relationship, while others find no significant link. Proposed mechanisms include mechanical loading, bone remodeling, and inflammation. Clinical strategies focus on maintaining bone health in OA and monitoring joint health in OP, with treatments like bisphosphonates and exercise. Understanding these interactions is crucial for developing integrated treatments to improve patient outcomes and quality of life. Further research is needed to clarify these complex mechanisms.
骨关节炎与骨质疏松症之间的相互作用:机制、影响和治疗考虑因素--叙述性综述。
这篇综合评论探讨了骨关节炎(OA)和骨质疏松症(OP)这两种老年人常见疾病之间的关系。骨关节炎会导致关节软骨退化和疼痛,而骨质疏松症则会因骨量减少而导致骨折。尽管病因不同,但这两种疾病都有年龄和遗传等风险因素。研究结果喜忧参半:一些研究显示,OA 患者的骨质密度(BMD)较高,表明两者之间存在反向关系,而另一些研究则发现两者之间没有明显联系。研究提出的机制包括机械负荷、骨重塑和炎症。临床策略侧重于维持 OA 患者的骨骼健康和监测 OP 患者的关节健康,并采用双膦酸盐和运动等治疗方法。了解这些相互作用对于开发综合疗法以改善患者预后和生活质量至关重要。要弄清这些复杂的机制,还需要进一步的研究。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Experimental gerontology
Ageing, Biochemistry, Geriatrics and Gerontology
CiteScore
6.70
自引率
0.00%
发文量
0
审稿时长
66 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


