Impact of commonly administered drugs on the progression of spinal cord injury: a systematic review
IF 5.4
Q1 MEDICINE, RESEARCH & EXPERIMENTAL
引用次数: 0
Abstract
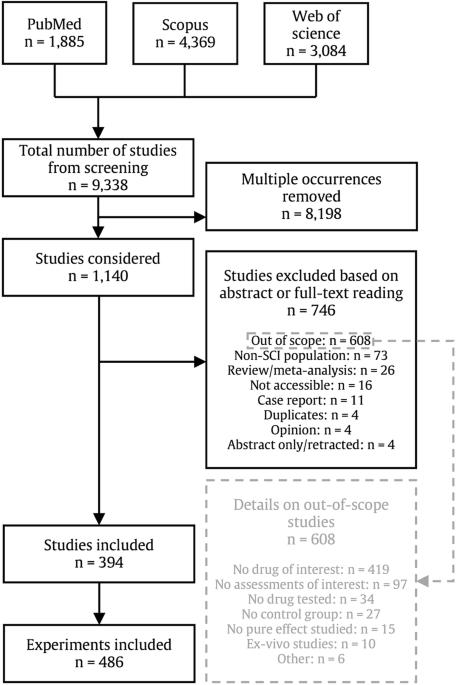
Complications arising from acute traumatic spinal cord injury (SCI) are routinely managed by various pharmacological interventions. Despite decades of clinical application, the potential impact on neurological recovery has been largely overlooked. This study aims to highlight commonly administered drugs with potential disease-modifying effects. This systematic literature review included studies referenced in PubMed, Scopus and Web of Science from inception to March 31st, 2021, which assess disease-modifying properties on neurological and/or functional recovery of drugs routinely administered following spinal cord injury. Drug effects were classified as positive, negative, mixed, no effect, or not (statistically) reported. Risk of bias was assessed separately for animal, randomized clinical trials, and observational human studies. We analyzed 394 studies conducting 486 experiments that evaluated 144 unique or combinations of drugs. 195 of the 464 experiments conducted on animals (42%) and one study in humans demonstrate positive disease-modifying properties on neurological and/or functional outcomes. Methylprednisolone, melatonin, estradiol, and atorvastatin are the most common drugs associated with positive effects. Two studies on morphine and ethanol report negative effects on recovery. Despite a large heterogeneity observed in study protocols, research from bed to bench and back to bedside provides an alternative approach to identify new candidate drugs in the context of SCI. Future research in human populations is warranted to determine if introducing drugs like melatonin, estradiol, or atorvastatin would contribute to enhancing neurological outcomes after acute SCI. Patients with spinal cord injury (SCI) are exposed to a wide range of medications treating health conditions arising as a consequence of the initial injury. The effect of providing patients with a large number of medications in the early period after injury, that is in the first days to weeks, on recovery from SCI, however, is typically not considered. This extensive and structured review of evidence from pre-clinical (animal) and clinical (human) studies quantifies these effects for the first time. 144 unique drugs or combinations of drugs previously reported to be administered in animal models or to patients with SCI have been studied for their effect on recovery across 486 distinct experiments. A small subset of drugs are associated with positive effects, and provide potential targets for further study to determine if they can be used to treat SCI. Bourguignon, Lukas et al. systematically review the effect of drugs commonly administered after traumatic spinal cord injury on the neurological recovery in both animal studies and humans. Extensive heterogeneity in study characteristics and results highlight the need for harmonization across the field but also the potential for drug repurposing.
常用药物对脊髓损伤进展的影响:系统综述。
背景:急性创伤性脊髓损伤(SCI)引起的并发症通常会通过各种药物干预来控制。尽管临床应用了几十年,但其对神经系统恢复的潜在影响在很大程度上被忽视了。本研究旨在强调具有潜在疾病调节作用的常用药物:本系统性文献综述包括 PubMed、Scopus 和 Web of Science 中引用的从开始到 2021 年 3 月 31 日的研究,这些研究评估了脊髓损伤后常规用药对神经和/或功能恢复的疾病调节特性。药物效应分为阳性、阴性、混合效应、无效应或未报告(统计)效应。分别评估了动物、随机临床试验和观察性人体研究的偏倚风险:我们分析了 394 项研究,共进行了 486 次实验,评估了 144 种独特药物或药物组合。在 464 项动物实验中,有 195 项(42%)和一项人体研究证明了药物对神经和/或功能结果具有积极的疾病调节作用。甲基强的松龙、褪黑素、雌二醇和阿托伐他汀是最常见的具有积极作用的药物。关于吗啡和乙醇的两项研究报告了对康复的负面影响:尽管在研究方案中观察到很大的异质性,但从床边到工作台再回到床边的研究为确定 SCI 候选新药提供了另一种方法。未来有必要在人群中开展研究,以确定引入褪黑素、雌二醇或阿托伐他汀等药物是否有助于改善急性 SCI 后的神经功能预后。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


