Insomnia treatment effects on negative emotionality among veterans in treatment for alcohol use disorder
Abstract
Background
Insomnia symptoms are pervasive and persistent in alcohol use disorder (AUD), though little is known about the mechanisms that underlie this association. We previously found that cognitive behavioral therapy for insomnia (CBT-I) reduced alcohol-related problems among veterans by improving insomnia severity (NCT03806491). In this planned secondary analysis of the same clinical trial data, we tested negative emotionality as one potential mechanism to explain this effect. Specifically, we tested the change in negative emotionality as a mediator of the association between change in insomnia symptoms and alcohol-related outcomes (craving, heavy drinking frequency, and alcohol-related problems).
Methods
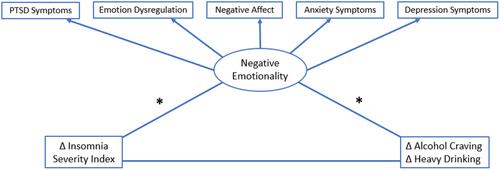
Participants were 67 veterans in treatment for AUD who also met the criteria for insomnia disorder (91% male, 84% White, average age = 46.3 years). Participants were randomized to five sessions of CBT-I or a single-session sleep hygiene control. Assessments occurred at baseline, immediately posttreatment (~6 weeks after baseline), and at 6-week follow-up. Measures included the Insomnia Severity Index, Penn Alcohol Craving Scale, Timeline Followback, and Short Inventory of Problems. We created a latent negative emotionality indicator based on five validated and reliable measures of negative emotionality.
Results
Contrary to hypotheses, CBT-I did not improve negative emotionality relative to sleep hygiene control. However, across both treatment conditions, decreases in insomnia symptoms from baseline to posttreatment were associated with concurrent decreases in negative emotionality, which in turn predicted reductions in alcohol craving and heavy drinking.
Conclusion
Negative emotionality may help explain links between insomnia symptoms and alcohol-related outcomes.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


