Association of depressive symptoms and incident chronic kidney disease in middle-aged and older adults
IF 4.1
2区 医学
Q1 PSYCHIATRY
引用次数: 0
Abstract
Background
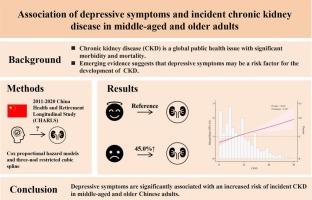
Emerging evidence suggests that depressive symptoms may be a risk factor for the development of Chronic kidney disease (CKD). This study aimed to investigate the association between depressive symptoms and the incidence of CKD in middle-aged and older Chinese adults.
Methods
We utilized data from the 2011–2020 China Health and Retirement Longitudinal Study (CHARLS). Depressive symptoms were assessed using the 10-item Center for Epidemiologic Studies Depression Scale (CES-D). Incident CKD was defined based on the estimated glomerular filtration rate ≤ 60 mL/min/m2 or self-reported. Cox proportional hazard models were used to estimate the hazard ratio (HR) and 95 % confidence intervals (95 % CI) for incident CKD, adjusting for potential confounders.
Results
Among the 10,996 participants without baseline CKD, 890 developed CKD during a median follow-up of 9.0 years. After adjusting for potential covariates, participants with depressive symptoms had a significantly higher risk of developing CKD compared to those without depressive symptoms (HR: 1.450; 95 % CI: 1.249–1.682). The association remained statistically significant when the CES-D was scored according to the severity of depressive symptoms, i.e., quintiles. A linear positive association between total CES-D score and risk of incident CKD was also found using restricted cubic spline regression (P for non-linearity = 0.114).
Conclusions
Depressive symptoms are significantly associated with an increased risk of incident CKD in middle-aged and older Chinese adults. These findings underscore the importance of mental health screening and interventions in preventing CKD in this population.
中老年人抑郁症状与慢性肾病发病率的关系。
背景:新的证据表明,抑郁症状可能是慢性肾脏病(CKD)发病的一个危险因素。本研究旨在调查中国中老年人抑郁症状与慢性肾脏病发病率之间的关系:我们利用了 2011-2020 年中国健康与退休纵向研究(CHARLS)的数据。抑郁症状采用 10 项流行病学研究中心抑郁量表(CES-D)进行评估。根据估计的肾小球滤过率≤ 60 mL/min/m2 或自我报告的情况来界定是否患有慢性肾功能衰竭。在对潜在混杂因素进行调整后,采用 Cox 比例危险模型来估算发生 CKD 的危险比(HR)和 95 % 置信区间(95 % CI):在 10996 名无基线 CKD 的参与者中,有 890 人在中位 9.0 年的随访期间患上了 CKD。在对潜在的协变量进行调整后,与无抑郁症状的参与者相比,有抑郁症状的参与者罹患慢性肾脏病的风险明显更高(HR:1.450;95 % CI:1.249-1.682)。如果根据抑郁症状的严重程度(即五分位数)对 CES-D 进行评分,这种关联在统计学上仍有意义。使用限制性三次样条回归法还发现,CES-D 总分与发生慢性肾脏病的风险呈线性正相关(非线性 P = 0.114):结论:抑郁症状与中国中老年人罹患慢性肾脏病的风险增加密切相关。结论:抑郁症状与中国中老年人发生慢性肾脏病的风险增加密切相关,这些发现强调了心理健康筛查和干预对预防中老年人慢性肾脏病的重要性。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

General hospital psychiatry
医学-精神病学
CiteScore
9.60
自引率
2.90%
发文量
125
审稿时长
20 days
期刊介绍:
General Hospital Psychiatry explores the many linkages among psychiatry, medicine, and primary care. In emphasizing a biopsychosocial approach to illness and health, the journal provides a forum for professionals with clinical, academic, and research interests in psychiatry''s role in the mainstream of medicine.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


