Comparison of pooled cohort equation and PREVENT™ risk calculator for statin treatment allocation
IF 4.9
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background and aims
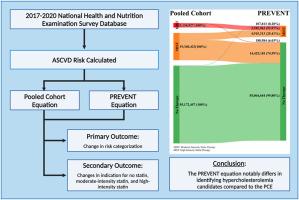
Effective hypercholesterolemia management is linked to lower all-cause and cardiovascular mortality. The 2018 AHA/ACC guidelines recommended using the Pooled Cohort Equations (PCE) for lipid management, but these may overestimate risk and be less accurate for certain racial groups. The AHA's new PREVENT equation, which omits race and includes cardiometabolic factors, aims to provide a more accurate risk assessment for a diverse population. However, it has not yet been applied to a nationally representative US population, and implementation guidelines are still lacking. Our study aimed to evaluate potential changes in hypercholesterolemia management for primary prevention by using the PREVENT equation instead of the PCE.
Methods
Analyzing pre-pandemic NHANES 2017–2020 data, participants aged 40–75 without prior lipid-lowering treatment or other compelling indication were identified for elevated risk (≥7.5 %) using the PCE and PREVENT equations. We assessed risk shifts and indications for statin therapy, comparing the two risk equations. NHANES guidelines with weighting were followed to obtain US nationally representative estimates.
Results
Out of 77, 647, 807 (unweighted = 2494) participants, 81.0 % had no change in risk. The PCE flagged 18.8 % (n = 14,614,094) of participants at elevated risk not identified by PREVENT, while 0.20 % (n = 107,813) were flagged only by PREVENT. Participants identified solely by the PCE were older, with higher systolic blood pressure and increased estimated glomerular filtration rates.
Indications for statin therapy were largely unchanged (81.0 %). PREVENT newly identified (0.20 %) for moderate-intensity therapy and none for high-intensity therapy. Participants qualifying for moderate intensity therapy by the PCE were reclassified to no therapy in 74.59 % of cases, while 25.41 % remained unchanged. Participants qualifying for high-intensity therapy by the PCE were reclassified to moderate therapy in 93.97 % of cases, and 6.03 % were reclassified to no therapy.
Conclusions
The PREVENT equation notably differs in identifying hypercholesterolemia candidates compared to the PCE. Its adoption would influence cardiovascular risk reduction therapy recommendations, emphasizing the need for comprehensive studies to understand its long-term impact and reevaluate the threshold of treatment strategies for improved patient outcomes.
用于他汀类药物治疗分配的汇集队列方程与 PREVENT™ 风险计算器的比较。
背景和目的:有效的高胆固醇血症管理与降低全因死亡率和心血管死亡率有关。2018 年 AHA/ACC 指南建议使用集合队列方程 (PCE) 进行血脂管理,但这些方程可能会高估风险,对某些种族群体的准确性较低。美国心脏病学会的新 PREVENT 方程省略了种族因素并包含了心脏代谢因素,旨在为不同人群提供更准确的风险评估。然而,该方程尚未应用于具有全国代表性的美国人群,也缺乏实施指南。我们的研究旨在评估使用 PREVENT 方程而非 PCE 进行一级预防时高胆固醇血症管理的潜在变化:通过分析大流行前的 NHANES 2017-2020 年数据,使用 PCE 和 PREVENT 方程确定了年龄在 40-75 岁、既往未接受过降脂治疗或无其他强制指征的参与者的高风险(≥7.5%)。我们对两种风险方程进行了比较,评估了他汀类药物治疗的风险转移和适应症。为了获得具有美国全国代表性的估计值,我们遵循了 NHANES 的加权指南:在 77 647 807(未加权 = 2494)名参与者中,81.0% 的风险没有变化。PCE标记了18.8%(n=14,614,094)未被PREVENT识别的高风险参与者,而0.20%(n=107,813)仅被PREVENT标记。仅通过 PCE 确定的参与者年龄较大,收缩压较高,估计肾小球滤过率较高。他汀类药物治疗的适应症基本未变(81.0%)。PREVENT 新发现(0.20%)可接受中等强度治疗的患者,没有发现可接受高强度治疗的患者。有 74.59% 符合 PCE 中度治疗条件的参与者被重新分类为无需治疗,25.41% 保持不变。93.97%的病例被重新分类为中度治疗,6.03%的病例被重新分类为无治疗:与 PCE 相比,PREVENT 方程在确定高胆固醇血症候选者方面存在显著差异。结论:与 PCE 相比,PREVENT 方程在确定高胆固醇血症候选者方面存在显著差异,它的采用将影响降低心血管风险疗法的建议,因此需要进行全面研究以了解其长期影响,并重新评估治疗策略的阈值,以改善患者的预后。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Atherosclerosis
医学-外周血管病
CiteScore
9.80
自引率
3.80%
发文量
1269
审稿时长
36 days
期刊介绍:
Atherosclerosis has an open access mirror journal Atherosclerosis: X, sharing the same aims and scope, editorial team, submission system and rigorous peer review.
Atherosclerosis brings together, from all sources, papers concerned with investigation on atherosclerosis, its risk factors and clinical manifestations. Atherosclerosis covers basic and translational, clinical and population research approaches to arterial and vascular biology and disease, as well as their risk factors including: disturbances of lipid and lipoprotein metabolism, diabetes and hypertension, thrombosis, and inflammation. The Editors are interested in original or review papers dealing with the pathogenesis, environmental, genetic and epigenetic basis, diagnosis or treatment of atherosclerosis and related diseases as well as their risk factors.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


