Elevations in interleukin-8 levels in individuals with alcohol use disorder and clinical insomnia symptoms
Abstract
Background
Insomnia commonly co-occurs with alcohol use disorder (AUD) and predicts poorer outcomes for those with AUD. Insomnia and AUD are individually associated with increases in systemic inflammation. Insomnia and inflammation both serve as risk factors for relapse in AUD. However, little is known about the relationship between insomnia and systemic inflammation in individuals with AUD. Therefore, the present study examined the relationship between the severity of insomnia symptoms and plasma levels of inflammatory cytokines in a sample of treatment-seeking individuals with an AUD.
Methods
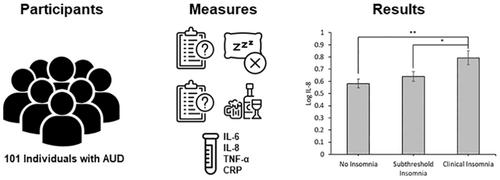
This secondary analysis included 101 (61M/40F) individuals with an AUD. Participants were categorized into groups based on their scores on the Insomnia Severity Index: no insomnia (n = 47), subthreshold insomnia (n = 37), and clinical insomnia (n = 17). Participants provided blood samples to measure plasma levels of four peripheral markers of inflammation (IL-6, IL-8, TNF-α, and CRP). Inflammatory marker levels were compared between groups. Interactive effects of sex and AUD severity were examined.
Results
There was a significant main effect of insomnia group on log IL-8 levels (F = 6.52, p = 0.002), such that individuals with AUD and clinical insomnia had higher log IL-8 levels compared to both the no insomnia and subthreshold insomnia groups (ps ≤ 0.05). Sex and AUD severity interacted with this relationship, such that men with clinical insomnia and AUD and individuals with severe AUD had higher log IL-8 levels. There were no significant effects of insomnia on IL-6, TNF-α, or CRP levels.
Conclusion
The present study identified a specific elevation in IL-8 levels in individuals with an AUD and clinical insomnia that was not identified in other markers of peripheral inflammation (IL-6, TNF-α, CRP). Sex and AUD severity interacted with insomnia symptoms, indicating that those with clinical insomnia and severe AUD or male sex may be the most vulnerable to the inflammatory consequences associated with AUD and clinical insomnia symptoms.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


