Detection of Rifampicin Resistance rpoB Gene Using GeneXpert MTB/RIF Assay in Pulmonary Tuberculosis Cases at Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia
Abstract
Background
Tuberculosis (TB) is a preventable and treatable disease leading to the second death globally. The evolution of drug resistance in Mycobacterium tuberculosis (MTB), particularly rifampicin resistance (RR), has hampered TB control efforts. Thus, this study aimed to provide information regarding the magnitude of MTB and rifampicin resistance among patients tested using the GeneXpert method.
Methods
A retrospective analysis was carried out at DTCSH. The study included TB registration logbook data from all patients who visited the hospital and were tested for MTB with the Xpert MTB/RIF assay from 2017 to 2024. The laboratory-based data were entered, cleaned, and analyzed using SPSS version 26 software. Multilogistic regression analysis was employed, and a p value ≤ 0.05 was considered statistically significant.
Results
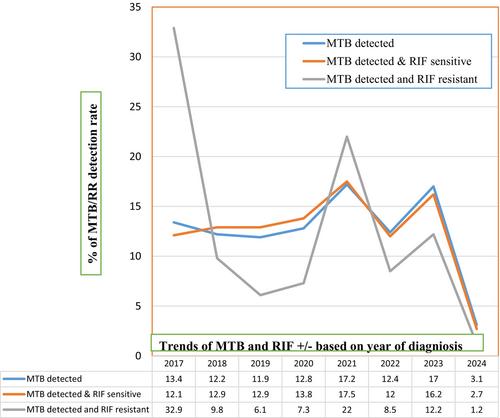
A total of 12,981 patient results were included, of which 8.9% (1160/12,981) were MTB-positive and 7.1% (82/1160) were RR. Individuals aged 15–29 years (AOR = 2.13; 95% CI = 1.55–2.93, p < 0.001), living in rural areas (AOR = 1.23; 95% CI = 1.08–1.41, p = 0.003), and HIV+ (AOR = 1.79; 95% CI = 1.48–2.33, p < 0.001) had a higher risk of developing tuberculosis. While RR was identified in 63.4% (52/82) of new, 24.4% (20/82) of re-treated, and 12.2% (10/82) of failed presumptive TB patients.
Conclusion
In this study, MTB and RR trends were high. Productive age groups, rural populations, and HIV patients were at risk. To lessen the burden of this contagious and fatal disease, it is recommended to increase early diagnosis of drug-resistant TB and enhance infection control.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


