Chronic glycemic control influences the relationship between acute perioperative dysglycemia and perioperative outcome
Abstract
Background
The objective of this study was to evaluate the impact of dysglycemia on perioperative outcomes, in patients with and without diabetes, and how prior glycemic control modifies these relationships.
Methods
Consecutive surgical patients admitted to six South Australian tertiary hospitals between 2017 and 2023 were included. Blood glucose levels within 48 h pre- and post-operatively were assessed in an adjusted analyses against a priori selected covariates. Dysglycemia metrics were hyperglycemia (>10.0 mmol/L), hypoglycemia (<4.0 mmol/L), glycemic variability (standard deviation of mean blood glucose >1.7 mmol/L), and stress hyperglycemic ratio (SHR). The primary outcome was hospital mortality.
Results
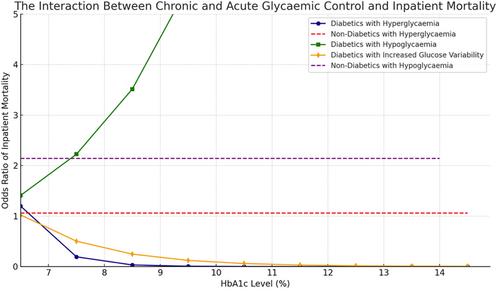
Of 52 145 patients, 7490 (14.4%) had recognized diabetes. Inpatient mortality was observed in 787 patients (1.5%), of which 150 (19.1%) had diabetes mellitus. Hyperglycemia was associated with increased mortality in patients with diabetes (odds ratio [OR] = 2.99, 95% CI: 1.63–5.67, p = 0.004) but not in non-diabetics, who instead had an increased odds of intensive care unit (ICU) admission if hyperglycemic (OR = 1.95, 95% CI: 1.40–2.72, p < 0.0001). Glycemic variability was associated with increased mortality in patients with diabetes (OR = 1.46, 95% CI: 1.05–2.01, p < 0.05) but not in non-diabetics. Preoperative glycemic control (HbA1c) attenuated both of these associations in a dose-dependent fashion. Hypoglycemia was associated with increased mortality in non-diabetics (OR = 2.14, 95% CI: 1.92–2.37, p < 0.001) but not in patients with diabetes.
Conclusions,
In surgical patients with diabetes, prior exposure to hyperglycemia attenuates the impact of perioperative hyperglycemia and glycemic variability on inpatient mortality and ICU admission. In patients without diabetes mellitus, all absolute thresholds of dysglycemia are associated with ICU admission, unlike those with diabetes, suggesting the need to use more relative measures such as the SHR.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


