International expert consensus statement on the diagnosis and management of congenital nephrogenic diabetes insipidus (arginine vasopressin resistance)
IF 28.6
1区 医学
Q1 UROLOGY & NEPHROLOGY
引用次数: 0
Abstract
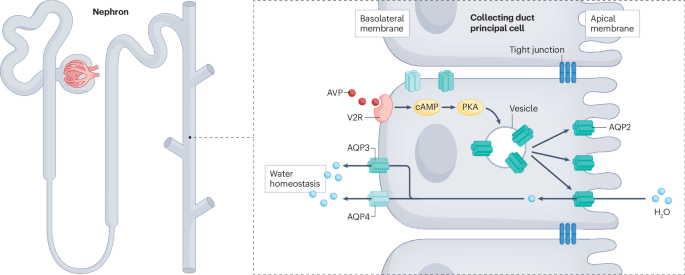
Congenital nephrogenic diabetes insipidus (NDI; also known as arginine vasopressin resistance) is a rare inherited disorder of water homeostasis, caused by insensitivity of the distal nephron to arginine vasopressin. Consequently, the kidney loses its ability to concentrate urine, which leads to polyuria, polydipsia and the risk of hypertonic dehydration. The diagnosis and management of NDI are very challenging and require an integrated, multidisciplinary approach. Here, we present 36 recommendations for diagnosis, treatment and follow-up in both children and adults, as well as emergency management, genetic counselling and family planning, for patients with NDI. These recommendations were formulated and graded by an international group of experts in NDI from paediatric and adult nephrology, urology and clinical genetics from the European Rare Kidney Disease Reference Network and the European Society of Paediatric Nephrology, as well as patient advocates, and were validated by a voting panel in a Delphi process. The goal of these recommendations is to provide guidance to health care professionals who care for patients with NDI and to patients and their families. In addition, we emphasize the need for further research on different aspects of this potentially life-threatening disorder to support the development of evidence-based guidelines in the future. Congenital nephrogenic diabetes insipidus is a rare but potentially life-threatening condition. This Consensus Statement provides clinical practice recommendations developed by the European Reference Network on Rare Kidney Diseases, the European Society for Paediatric Nephrology and patient advocates to support clinicians in the diagnosis, treatment and genetic counselling of children and adults with nephrogenic diabetes insipidus.

关于先天性肾源性尿崩症(精氨酸加压素抵抗)诊断和管理的国际专家共识声明
先天性肾源性糖尿病(NDI,又称精氨酸加压素抵抗)是一种罕见的遗传性水平衡失调症,由远端肾小球对精氨酸加压素不敏感引起。因此,肾脏失去了浓缩尿液的能力,导致多尿、多饮和高渗性脱水的风险。NDI 的诊断和管理非常具有挑战性,需要多学科综合方法。在此,我们针对儿童和成人 NDI 患者的诊断、治疗和随访以及应急管理、遗传咨询和计划生育提出了 36 项建议。这些建议由来自欧洲罕见肾脏病参考网络和欧洲儿科肾脏病学会的儿科和成人肾脏病学、泌尿学和临床遗传学领域的 NDI 国际专家组以及患者权益倡导者共同制定和分级,并通过德尔菲程序由投票小组进行验证。这些建议旨在为护理 NDI 患者的医护人员以及患者及其家属提供指导。此外,我们还强调有必要对这种可能危及生命的疾病的不同方面进行进一步研究,以支持未来循证指南的制定。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Reviews Nephrology
医学-泌尿学与肾脏学
CiteScore
39.00
自引率
1.20%
发文量
127
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Nephrology aims to be the premier source of reviews and commentaries for the scientific communities it serves.
It strives to publish authoritative, accessible articles.
Articles are enhanced with clearly understandable figures, tables, and other display items.
Nature Reviews Nephrology publishes Research Highlights, News & Views, Comments, Reviews, Perspectives, and Consensus Statements.
The content is relevant to nephrologists and basic science researchers.
The broad scope of the journal ensures that the work reaches the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


