Genetic risk score for coronary artery calcification and its predictive ability for coronary artery disease
IF 4.3
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Aim
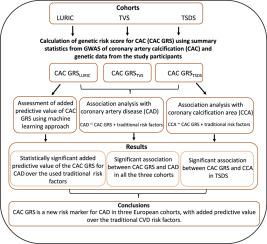
The modest added predictive value of the existing genetic risk scores (GRSs) for coronary artery disease (CAD) could be partly due to missing genetic components, hidden in the genetic architecture of intermediate phenotypes such as coronary artery calcification (CAC). In this study, we investigated the predictive ability of CAC GRS for CAD.
Materials and methods
We investigated the association of CAC GRSs with CAD and coronary calcification among the participants in the Ludwigshafen Risk and Cardiovascular Health study (LURIC) (n = 2742), the Tampere Vascular Study (TVS) (n = 133), and the Tampere Sudden Death Study (TSDS) (n = 660) using summary data from the largest multi-ancestry GWAS meta-analysis of CAC to date. Added predictive value of the CAC GRS over the traditional CVD risk factors as well as metaGRS, a GRS for CAD constructed with 1.7 million genetic variants, was tested with standard train–test machine learning approach using the LURIC data, which had the largest sample size.
Results
CAC GRS was significantly associated with CAD in LURIC (OR=1.41, 95 % CI [1.28–1.55]), TVS (OR=1.79, 95 % CI [1.05–3.21]) as well as in TSDS (OR=4.20, 95 % CI [1.74–10.52]). CAC GRS showed strong association with calcification areas in left (OR=1.78, 95 % CI [1.16–2.74]) and right (OR=1.71, 95 % CI [1.98–2.67]) coronary arteries. There was statistically significant added predictive value of the CAC GRS for CAD over the used traditional CVD risk factors (AUC 0.734 vs 0.717, p-value = 0.02). Furthermore, CAC GRS improved the prediction accuracy for CAD when combined with metaGRS.
Conclusions
This study showed that CAC GRS is a new risk marker for CAD in three European cohorts, with added predictive value over the traditional CVD risk factors.
冠状动脉钙化遗传风险评分及其对冠状动脉疾病的预测能力
目的现有遗传风险评分(GRSs)对冠状动脉疾病(CAD)的预测价值不高,部分原因可能是隐藏在冠状动脉钙化(CAC)等中间表型的遗传结构中的遗传成分缺失。在这项研究中,我们调查了 CAC GRS 对 CAD 的预测能力。材料与方法我们利用迄今为止最大的 CAC 多宗族 GWAS meta 分析的汇总数据,调查了路德维希港风险与心血管健康研究(LURIC)(n = 2742)、坦佩雷血管研究(TVS)(n = 133)和坦佩雷猝死研究(TSDS)(n = 660)参与者的 CAC GRS 与 CAD 和冠状动脉钙化的关联。利用样本量最大的 LURIC 数据,采用标准的训练-测试机器学习方法,测试了 CAC GRS 相对于传统心血管疾病风险因素以及元 GRS(用 170 万个基因变异构建的 CAD GRS)的预测价值。结果在 LURIC(OR=1.41,95 % CI [1.28-1.55])、TVS(OR=1.79,95 % CI [1.05-3.21])和 TSDS(OR=4.20,95 % CI [1.74-10.52])中,CAC GRS 与 CAD 显著相关。CAC GRS 显示与左冠状动脉(OR=1.78,95 % CI [1.16-2.74])和右冠状动脉(OR=1.71,95 % CI [1.98-2.67])的钙化面积密切相关。与使用的传统心血管疾病风险因素相比,CAC GRS 对 CAD 的预测值有明显的统计学意义(AUC 0.734 vs 0.717,p 值 = 0.02)。结论这项研究表明,在三个欧洲队列中,CAC GRS 是一种新的心血管疾病风险标志物,与传统的心血管疾病风险因素相比,具有更高的预测价值。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

American journal of preventive cardiology
Cardiology and Cardiovascular Medicine
CiteScore
6.60
自引率
0.00%
发文量
0
审稿时长
76 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


