Multidimensional phenotyping to distinguish among central (CSA), obstructive (OSA) and co-existing central and obstructive sleep apnea (CSA-OSA) phenotypes in real-world data
IF 3.8
2区 医学
Q1 CLINICAL NEUROLOGY
引用次数: 0
Abstract
Purpose
When navigating the landscape of obstructive sleep apnea (OSA), central sleep apnea (CSA) and intersection of the two diseases (co-existing CSA-OSA), there are significant knowledge gaps. Data are scarce regarding the respective prevalence and differences in clinical presentation of the three conditions. One major issue for characterization of the prevalence of the different sleep apnea entities is the scoring of central versus obstructive hypopneas which is not included in the routine practice of many sleep laboratories.
Method
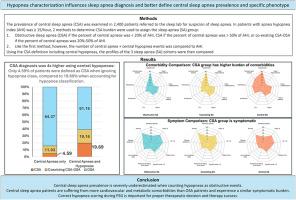
We prospectively assessed multidomain symptoms and collected data on comorbidities, medications and treatment indications in a large monocentric real-life dataset (n > 2400) of patients referred for suspicion of sleep apnea. We have systematically distinguished central versus obstructive hypopneas to define OSA, CSA and co-existing CSA-OSA.
Results
When CSA was defined by the proportion of central apneas (and hypopneas were considered obstructive by default), the prevalence of CSA was 4.59 % (co-existing CSA-OSA: 11.03 %, and OSA: 84.37 %). When the distinction between obstructive and central hypopneas was used to classify the sleep disordered breathing, the prevalence of CSA was fourfold higher at 19.69 % (co-existing: 19.16 %, OSA: 61.16 %). The burden of cardiovascular and metabolic comorbidities was the highest in the CSA and co-existing sleep apnea subgroups. The three sleep apnea groups exhibited different constellations of symptoms but most of the patients with CSA, co-existing and OSA were symptomatic after comprehensive evaluation. The CSA group exhibited the most severe disturbances in sleep architecture on polysomnography. Therapeutic indications differed depending on the subtype of respiratory events.
Conclusion
Our findings imply that not differentiating between central and obstructive hypopneas will underestimate the severity of central sleep disordered breathing abnormalities that mislead therapeutic decisions and might limit improvements in quality of life and sleepiness that are expected in appropriately treated patients with CSA.
通过多维表型分析,在真实世界数据中区分中枢性(CSA)、阻塞性(OSA)以及同时存在的中枢性和阻塞性睡眠呼吸暂停(CSA-OSA)表型
目的在研究阻塞性睡眠呼吸暂停(OSA)、中枢性睡眠呼吸暂停(CSA)以及这两种疾病的交集(并存的 CSA-OSA)时,存在很大的知识差距。关于这三种疾病各自的患病率和临床表现差异的数据十分匮乏。我们在一个大型单中心真实生活数据集中(n > 2400)对因怀疑睡眠呼吸暂停而转诊的患者进行了前瞻性的多领域症状评估,并收集了有关合并症、药物和治疗适应症的数据。我们系统地区分了中枢性和阻塞性低通气,从而定义了 OSA、CSA 和并存的 CSA-OSA。结果当根据中枢性呼吸暂停的比例定义 CSA 时(低通气默认为阻塞性),CSA 的患病率为 4.59%(并存的 CSA-OSA 为 11.03%,OSA 为 84.37%)。如果使用阻塞性和中枢性低通气来对睡眠呼吸障碍进行分类,则 CSA 的患病率要高出四倍,为 19.69 %(并存 CSA:19.16 %,OSA:61.16 %)。在 CSA 和并存睡眠呼吸暂停亚组中,心血管和代谢合并症的负担最重。三组睡眠呼吸暂停患者表现出不同的症状组合,但经过综合评估后,大部分 CSA、并存和 OSA 患者均无症状。CSA 组在多导睡眠图上显示出最严重的睡眠结构紊乱。结论我们的研究结果表明,不区分中枢性低通气和阻塞性低通气会低估中枢性睡眠呼吸障碍异常的严重程度,从而误导治疗决策,并可能限制 CSA 患者在接受适当治疗后生活质量和嗜睡程度的改善。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Sleep medicine
医学-临床神经学
CiteScore
8.40
自引率
6.20%
发文量
1060
审稿时长
49 days
期刊介绍:
Sleep Medicine aims to be a journal no one involved in clinical sleep medicine can do without.
A journal primarily focussing on the human aspects of sleep, integrating the various disciplines that are involved in sleep medicine: neurology, clinical neurophysiology, internal medicine (particularly pulmonology and cardiology), psychology, psychiatry, sleep technology, pediatrics, neurosurgery, otorhinolaryngology, and dentistry.
The journal publishes the following types of articles: Reviews (also intended as a way to bridge the gap between basic sleep research and clinical relevance); Original Research Articles; Full-length articles; Brief communications; Controversies; Case reports; Letters to the Editor; Journal search and commentaries; Book reviews; Meeting announcements; Listing of relevant organisations plus web sites.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


