Internal carotid artery dissection in a patient with Parkinson's disease after COVID-19 infection
Q3 Neuroscience
引用次数: 0
Abstract
Background
Internal carotid artery (ICA) dissection is a relatively rare cause of acute ischemic stroke. Stretching and compression of ICA due to sudden acceleration, deceleration, and rotational forces are risk factors for ICA dissection. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is believed to trigger an inflammatory response that exacerbates endothelial dysfunction and leads to arterial dissection. Although levodopa-induced cervical dyskinesia in Parkinson's disease often manifests as choreiform movement, dissection has not been reported in such patients.
Case presentation
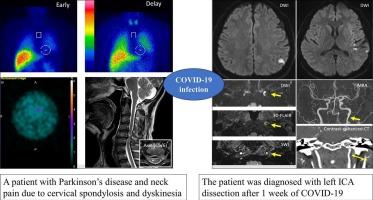
A 51-year-old man with Parkinson's disease (PD) presented with gradually worsening neck pain and transient aphasia 1 week after mild coronavirus disease 2019 (COVID-19) infection. The patient already had neck pain due to cervical spondylosis and presented with levodopa-induced cervical dyskinesia. Magnetic resonance imaging revealed acute ischemic stroke in the left parietal lobe and an intramural hematoma with an area of stenosis in the left ICA. The patient was diagnosed with left ICA dissection.
Conclusions
COVID-19 infection can cause vessel wall vulnerability. Although patients with PD often have neck pain, ICA dissection should be considered a differential diagnosis if the patient has a recent history of COVID-19.
一名帕金森病患者感染 COVID-19 后发生颈内动脉夹层
背景颈内动脉(ICA)夹层是导致急性缺血性卒中的一个相对罕见的原因。突然的加速、减速和旋转力导致的颈内动脉拉伸和压迫是导致颈内动脉夹层的危险因素。严重急性呼吸系统综合征冠状病毒 2(SARS-CoV-2)被认为会引发炎症反应,加剧内皮功能障碍,导致动脉夹层。尽管左旋多巴诱发的帕金森病颈部运动障碍通常表现为舞蹈样运动,但尚未有此类患者出现动脉夹层的报道。病例介绍一名 51 岁的帕金森病(PD)男性患者在轻度感染 2019 年冠状病毒病(COVID-19)一周后出现逐渐加重的颈部疼痛和一过性失语。患者原本就有颈椎病导致的颈部疼痛,并出现左旋多巴诱发的颈部运动障碍。磁共振成像显示,患者左顶叶急性缺血性卒中,左侧 ICA 存在壁内血肿和狭窄区域。结论COVID-19感染可导致血管壁脆弱。尽管PD患者常常伴有颈部疼痛,但如果患者近期有COVID-19病史,则应将ICA夹层视为鉴别诊断。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

eNeurologicalSci
Neuroscience-Neurology
CiteScore
3.50
自引率
0.00%
发文量
45
审稿时长
62 days
期刊介绍:
eNeurologicalSci provides a medium for the prompt publication of original articles in neurology and neuroscience from around the world. eNS places special emphasis on articles that: 1) provide guidance to clinicians around the world (Best Practices, Global Neurology); 2) report cutting-edge science related to neurology (Basic and Translational Sciences); 3) educate readers about relevant and practical clinical outcomes in neurology (Outcomes Research); and 4) summarize or editorialize the current state of the literature (Reviews, Commentaries, and Editorials). eNS accepts most types of manuscripts for consideration including original research papers, short communications, reviews, book reviews, letters to the Editor, opinions and editorials. Topics considered will be from neurology-related fields that are of interest to practicing physicians around the world. Examples include neuromuscular diseases, demyelination, atrophies, dementia, neoplasms, infections, epilepsies, disturbances of consciousness, stroke and cerebral circulation, growth and development, plasticity and intermediary metabolism. The fields covered may include neuroanatomy, neurochemistry, neuroendocrinology, neuroepidemiology, neurogenetics, neuroimmunology, neuroophthalmology, neuropathology, neuropharmacology, neurophysiology, neuropsychology, neuroradiology, neurosurgery, neurooncology, neurotoxicology, restorative neurology, and tropical neurology.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


