Cardiac power output associated with hospitalization and mortality in coronary artery disease patients at stage B heart failure
IF 2.5
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
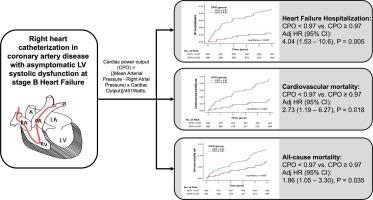
Cardiac power output (CPO) predicts outcomes in advanced heart failure (HF) and cardiogenic shock, but its role in early HF stages is unclear. This study assessed the prognostic value of CPO in coronary artery disease patients with asymptomatic left ventricular systolic dysfunction (ALVSD) at stage B HF.
Methods
We conducted a retrospective analysis of coronary artery disease patients who underwent coronary and pulmonary artery catheterization between 2006 and 2016. Stage B HF with ALVSD was defined as left ventricular ejection fraction < 50 %, without HF symptoms, signs, or prior HF hospitalization. CPO was derived from invasive hemodynamic parameters. Endpoints included HF hospitalization, cardiovascular mortality, and all-cause mortality over a 5-year follow-up.
Results
A total of 783 coronary artery disease patients with ALVSD at stage B HF were enrolled. Incidence rates (per 1000 person-years) were 13.9 for HF hospitalization, 14.5 for cardiovascular mortality, and 23.7 for all-cause mortality.Multivariate analysis adjusting for covariates demonstrated that CPO was independent associated with all endpoints. Patients with a low CPO (<0.97 Watts) were at significantly higher risk for HF hospitalization (adjusted hazard ratio [HR]: 4.04; 95 % CI: 1.53 – 10.6; p = 0.005), cardiovascular mortality (adjusted HR: 2.73; 95 % CI: 1.19 – 6.27; p = 0.018), and all-cause mortality (adjusted HR: 1.86; 95 % CI: 1.05 – 3.30; p = 0.035) compared to those with higher CPO, regardless of subgroup classification.
Conclusion
Resting CPO in patients with ALVSD is significantly associated with adverse events, including HF hospitalization and mortality, highlighting its value in early-stage HF management.
冠心病 B 期心力衰竭患者的心脏动力输出与住院和死亡率的关系
背景心脏动力输出(CPO)可预测晚期心力衰竭(HF)和心源性休克的预后,但其在HF早期阶段的作用尚不明确。本研究评估了 CPO 在无症状左室收缩功能障碍(ALVSD)的 B 期 HF 冠心病患者中的预后价值。方法我们对 2006 年至 2016 年间接受冠状动脉和肺动脉导管检查的冠心病患者进行了回顾性分析。伴有 ALVSD 的 B 期高血压定义为左心室射血分数 < 50%,无高血压症状、体征或既往高血压住院治疗。CPO来自有创血液动力学参数。终点包括 5 年随访期间的高频住院率、心血管死亡率和全因死亡率。调整协变量后进行的多变量分析表明,CPO 与所有终点均无关联。低 CPO(<0.97 瓦特)患者的心房颤动住院风险(调整后危险比 [HR]:4.04;95 % CI:1.53 - 10.6;p = 0.005)、心血管死亡率(调整后危险比:2.73;95 % CI:1.19 - 6.27;p = 0.018)和全因死亡率(调整后危险比:1.结论ALVSD 患者静注 CPO 与不良事件(包括 HF 住院和死亡率)显著相关,突出了其在早期 HF 管理中的价值。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

IJC Heart and Vasculature
Medicine-Cardiology and Cardiovascular Medicine
CiteScore
4.90
自引率
10.30%
发文量
216
审稿时长
56 days
期刊介绍:
IJC Heart & Vasculature is an online-only, open-access journal dedicated to publishing original articles and reviews (also Editorials and Letters to the Editor) which report on structural and functional cardiovascular pathology, with an emphasis on imaging and disease pathophysiology. Articles must be authentic, educational, clinically relevant, and original in their content and scientific approach. IJC Heart & Vasculature requires the highest standards of scientific integrity in order to promote reliable, reproducible and verifiable research findings. All authors are advised to consult the Principles of Ethical Publishing in the International Journal of Cardiology before submitting a manuscript. Submission of a manuscript to this journal gives the publisher the right to publish that paper if it is accepted. Manuscripts may be edited to improve clarity and expression.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


