Recent advances in the diagnosis and management of neuropsychiatric lupus
IF 29.4
1区 医学
Q1 RHEUMATOLOGY
引用次数: 0
Abstract
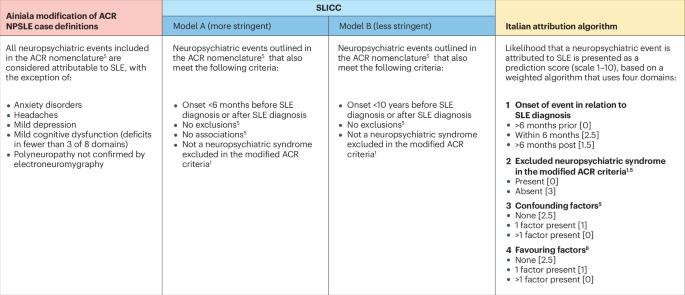
Neuropsychiatric manifestations of systemic lupus erythematosus (SLE) are common and frequently associated with a substantial negative impact on health outcomes. The pathogenesis of neuropsychiatric SLE (NPSLE) remains largely unknown, but a single pathogenic mechanism is unlikely to be responsible for the heterogeneous array of clinical manifestations, and a combination of inflammatory and ischaemic mechanistic pathways have been implicated. Currently, valid and reliable biomarkers for the diagnosis of NPSLE are lacking, and differentiating NPSLE from nervous system dysfunction not caused by SLE remains a major challenge for clinicians. However, correct attribution is essential to ensure timely institution of appropriate treatment. In the absence of randomized clinical trials on NPSLE, current treatment strategies are derived from clinical experience with different therapeutic modalities and their efficacy in the management of other manifestations of SLE or of neuropsychiatric disease in non-SLE populations. This Review describes recent advances in the understanding of NPSLE that can inform diagnosis and management, as well as unanswered questions that necessitate further research. Neuropsychiatric manifestations of systemic lupus erythematosus (SLE) are common and negatively impact health. Diagnosing neuropsychiatric SLE is challenging owing to a lack of reliable biomarkers, and current treatments rely on clinical experience. This Review covers recent clinical advances in this area and emphasizes the need for further research.

神经精神狼疮诊断和管理的最新进展
系统性红斑狼疮(SLE)的神经精神表现很常见,而且经常会对健康产生严重的负面影响。神经精神系统性红斑狼疮(NPSLE)的发病机制在很大程度上仍然未知,但单一的致病机制不太可能导致一系列不同的临床表现,炎症和缺血性机制途径的结合已被认为是其中的一个因素。目前,诊断非系统性红斑狼疮还缺乏有效可靠的生物标志物,如何将非系统性红斑狼疮与非系统性红斑狼疮引起的神经系统功能障碍区分开来仍然是临床医生面临的一大挑战。然而,正确的归因对于确保及时进行适当的治疗至关重要。由于缺乏有关非系统性红斑狼疮的随机临床试验,目前的治疗策略是根据不同治疗模式的临床经验及其在治疗系统性红斑狼疮的其他表现或非系统性红斑狼疮人群的神经精神疾病中的疗效而得出的。本综述介绍了在了解非系统性红斑狼疮方面取得的最新进展,这些进展可为诊断和治疗提供依据,同时也介绍了需要进一步研究的未解之谜。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Reviews Rheumatology
医学-风湿病学
CiteScore
29.90
自引率
0.90%
发文量
137
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Rheumatology is part of the Nature Reviews portfolio of journals. The journal scope covers the entire spectrum of rheumatology research. We ensure that our articles are accessible to the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


