Correlation Between Temporomandibular Joint Disc Perforation and Degenerative Joint Changes: A CBCT and Clinical Analysis
Abstract
Objectives
To analyse the correlation between temporomandibular joint (TMJ) disc perforation and degenerative joint changes (DJC) on cone-beam computed tomography (CBCT) and related factors.
Study Design
A total of 238 female patients with anterior disc displacement without reduction (ADDwoR), accounting for 348 affected joints, requiring TMJ disc open anchorage surgery were included in the study conducted from June 2021 to August 2022. Following TMJ disc open anchorage surgery, patients were divided into two groups: disc perforation (DP) and disc non-perforation (DNP). CBCT was utilised to assess different grades of condyle and articular eminence degenerative changes, and comparisons were made between the two groups regarding DJC and clinically relevant factors.
Results
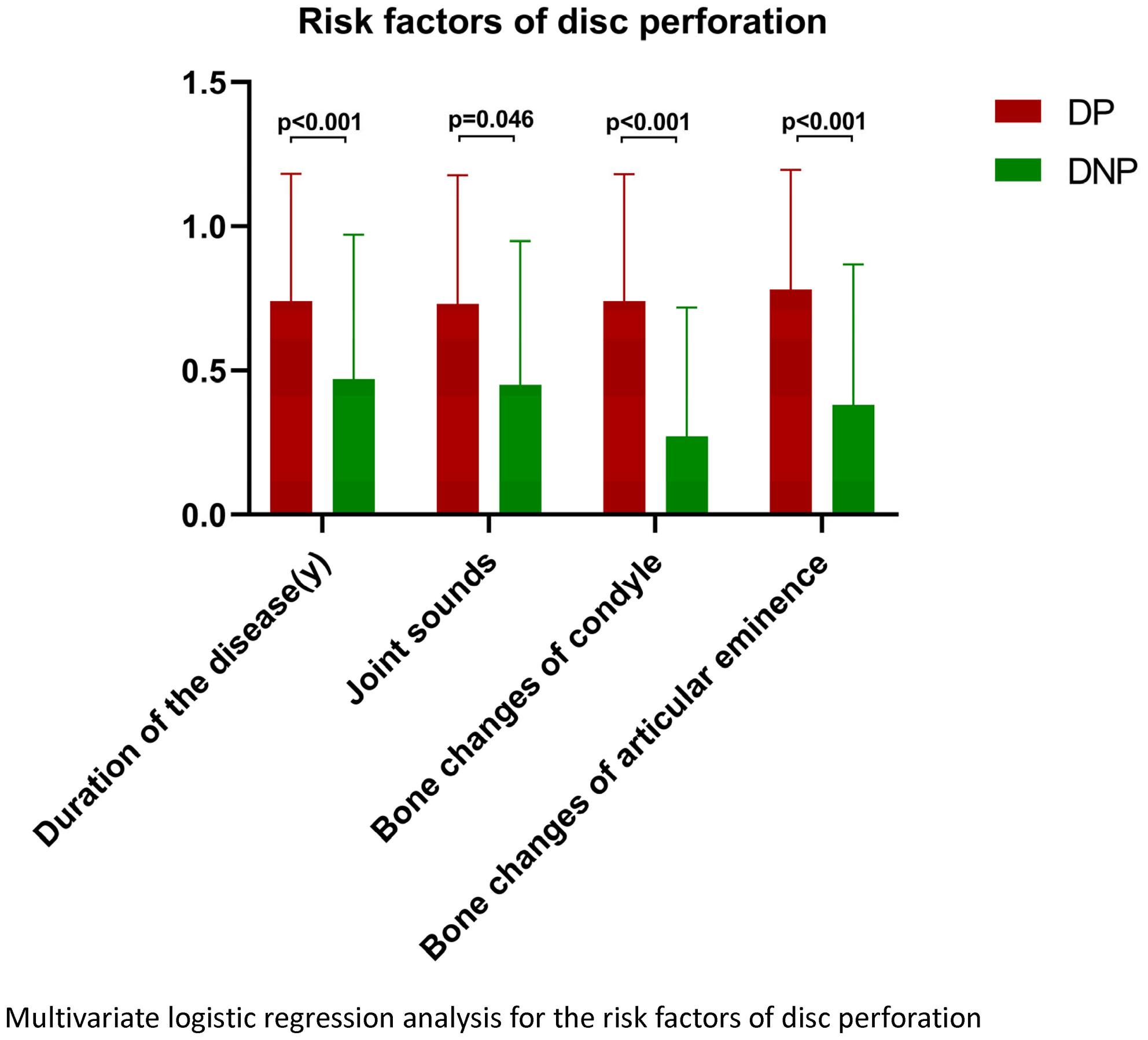
In comparison with the DNP group, the DP group exhibited statistically significant differences in mid- and late-stage condyle bone degenerative changes and bone alterations of the articular eminence (odds ratio [OR] = 7.822; 95% CI [4.438–13.785]; p < 0.001 and OR = 5.575; 95% CI [3.128–9.936]; p < 0.001). Additionally, persistent joint sounds (OR = 1.932; 95% CI [1.011–3.691]; p = 0.046) and longer disease duration (OR = 4.901; 95% CI [2.395–10.028]; p < 0.001) demonstrated statistically significant differences. However, no significant differences were observed between the two groups in terms of age, joint pain and limited mouth opening.
Conclusions
Bone degeneration changes in TMJ CBCT images are a high possible risk factor for DP. With an escalation in the degree of condyle degeneration, the risk of DP may increased correspondingly. Persistent joint sounds and extended duration of the disease were also confirmed to be noteworthy clinical risks of DP.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


