Advanced vascular aging and outcomes after acute ischemic stroke: a systematic review and meta-analysis
IF 2.7
4区 医学
Q2 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
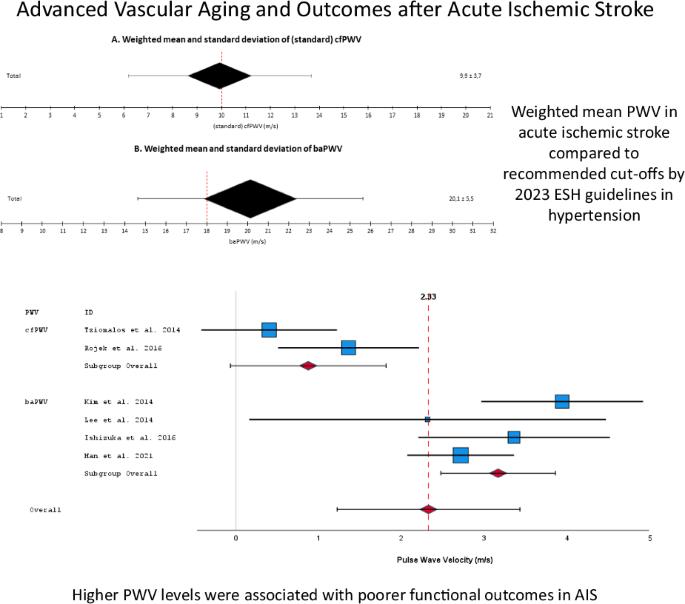
Pulse wave velocity (PWV) is as a reliable marker of arterial stiffness and vascular aging, surpassing traditional risk factors in predicting detrimental cardiovascular events. The present meta-analysis aims to investigate PWV thresholds and assess its prognostic value in outcomes of acute ischemic stroke (AIS). A search was conducted in PubMed, Cochrane, Web of Science, and Scopus for studies published up to January 2024, focusing on patients admitted with AIS, wherein arterial stiffness was assessed through PWV measurements during hospitalization. Identified studies reported PWV values in individuals with both favorable and unfavorable outcomes at the end of follow-up. Initially, 35 eligible studies provided data for weighted mean baPWV (11,953 AIS patients) and cfPWV (2,197 AIS patients) calculations. The average age was 67 years, with approximately 60% male, 67% hypertensive, 30% diabetic and 30% smoker participants. The weighted mean systolic blood pressure was approximately 150 mmHg. In AIS patients, the mean PWV was 10 m/s for standard cfPWV and 20 m/s for baPWV. Nine cohort studies (6,006 AIS patients) were included in the quantitative analysis of clinical outcomes. Higher PWV levels were associated with poorer functional outcomes (2.3 m/s higher, 95%CI:1.2–3.4, p < 0.001; I2 = 87.4%). AIS patients with arterial stiffness/vascular aging (higher PWV) had approximately 46.2% increased risk of poor functional outcome, 12.7% higher risk of mortality, 13.9% greater risk of major adverse cardiovascular events, and 13.9% greater risk of stroke recurrence over the long term compared to those without arterial stiffness. Advanced vascular aging, as indicated by PWV, significantly predicts adverse outcomes in AIS patients. Integrating the assessment of vascular aging into clinical practice can improve risk perception in these patients.
血管晚期老化与急性缺血性中风后的预后:系统回顾与荟萃分析。
脉搏波速度(PWV)是动脉僵化和血管老化的可靠标志,在预测有害心血管事件方面超过了传统的风险因素。本荟萃分析旨在研究脉搏波速度阈值并评估其在急性缺血性卒中(AIS)预后中的价值。我们在 PubMed、Cochrane、Web of Science 和 Scopus 上检索了截至 2024 年 1 月发表的研究,这些研究主要针对 AIS 患者,在住院期间通过脉搏波速度测量评估动脉僵化。已确定的研究报告了随访结束时有利和不利结果患者的脉搏波速度值。最初,35 项符合条件的研究提供了数据,用于加权平均 baPWV(11953 名 AIS 患者)和 cfPWV(2197 名 AIS 患者)的计算。参与者的平均年龄为 67 岁,男性约占 60%,高血压患者占 67%,糖尿病患者占 30%,吸烟者占 30%。加权平均收缩压约为 150 毫米汞柱。在 AIS 患者中,标准 cfPWV 的平均脉搏波速度为 10 m/s,baPWV 为 20 m/s。九项队列研究(6,006 名 AIS 患者)被纳入临床结果的定量分析。脉搏波速度水平越高,功能预后越差(高出 2.3 m/s,95%CI:1.2-3.4,p 2 = 87.4%)。与无动脉僵化的患者相比,动脉僵化/血管老化(脉搏波速度较高)的 AIS 患者长期功能预后不良的风险增加了约 46.2%,死亡率增加了 12.7%,主要不良心血管事件的风险增加了 13.9%,中风复发的风险增加了 13.9%。脉搏波速度(PWV)显示的血管高度老化可显著预测 AIS 患者的不良预后。将血管老化评估纳入临床实践可以改善这些患者的风险意识。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Journal of Human Hypertension
医学-外周血管病
CiteScore
5.20
自引率
3.70%
发文量
126
审稿时长
6-12 weeks
期刊介绍:
Journal of Human Hypertension is published monthly and is of interest to health care professionals who deal with hypertension (specialists, internists, primary care physicians) and public health workers. We believe that our patients benefit from robust scientific data that are based on well conducted clinical trials. We also believe that basic sciences are the foundations on which we build our knowledge of clinical conditions and their management. Towards this end, although we are primarily a clinical based journal, we also welcome suitable basic sciences studies that promote our understanding of human hypertension.
The journal aims to perform the dual role of increasing knowledge in the field of high blood pressure as well as improving the standard of care of patients. The editors will consider for publication all suitable papers dealing directly or indirectly with clinical aspects of hypertension, including but not limited to epidemiology, pathophysiology, therapeutics and basic sciences involving human subjects or tissues. We also consider papers from all specialties such as ophthalmology, cardiology, nephrology, obstetrics and stroke medicine that deal with the various aspects of hypertension and its complications.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


