Prevalence, correlates, and health indicators associated with meal-skipping among middle-aged and older adults in Thailand: A national longitudinal study
Abstract
Aim
The purpose of this longitudinal study was to evaluate the prevalence and correlates of and the factors contributing to meal-skipping in middle-aged and older adults in Thailand.
Methods
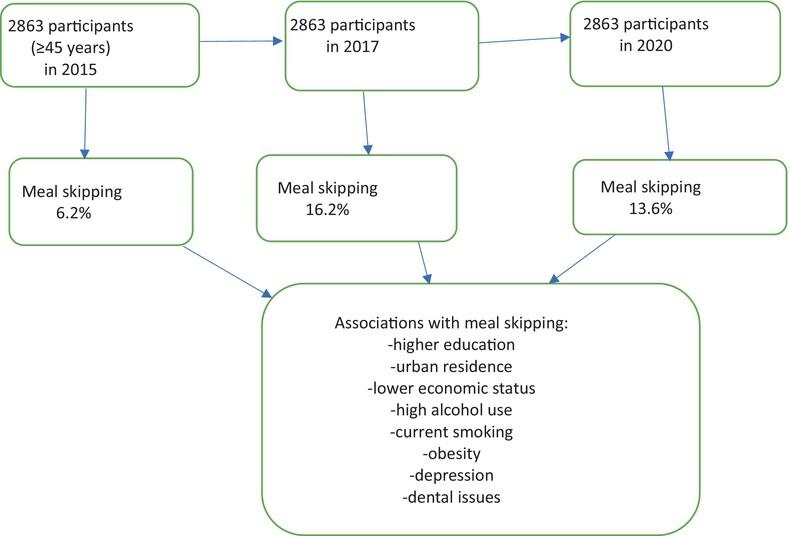
We examined prospective cohort data from three consecutive waves of the Health, Aging and Retirement in Thailand (HART) study (analytic sample size = 2863) for participants 45 years of age and older. Meal-skipping was assessed with a one- and two-day recall of breakfast, lunch, and dinner. We used generalized estimating equations analysis to evaluate the longitudinal relationships between sociodemographic, lifestyle, and health indicators and meal-skipping between 2015 (wave 1), 2017 (wave 2), and 2020 (wave 3). Furthermore, binary logistic regression was used to establish the longitudinal association between meal-skipping and the incidence of multiple chronic conditions.
Results
The prevalence of meal-skipping was 6.2% in 2015, 16.2% in 2017, and 13.6% in 2020, and across study years the highest proportion of meal skipping was for lunch (6.0%), followed by breakfast (4.6%), and dinner (2.8%). In the final model, sociodemographic factors (higher education, urban residence, and lower subjective economic status), lifestyle factors (high alcohol use, current smoking, and obesity class II), and health indicators (probable depression and wearing dentures) were positively associated with meal-skipping. In the adjusted logistic regression models, compared with no meal-skipping, meal-skipping in 2–3 study waves was associated with incident obesity and incident probable depression.
Conclusion
Skipping meals was linked to a number of lifestyle variables and indicators of physical and mental illness. Geriatr Gerontol Int 2024; 24: 1196–1202.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


