Association of age at diagnosis of type 2 diabetes mellitus with the risks of the morbidity of cardiovascular disease, cancer and all-cause mortality: Evidence from a real-world study with a large population-based cohort study
IF 6.1
3区 医学
Q1 ENDOCRINOLOGY & METABOLISM
引用次数: 0
Abstract
Aims
To investigate the impact of diagnosis age of type 2 diabetes mellitus (T2DM) on subsequent adverse outcomes within the Chinese population.
Methods
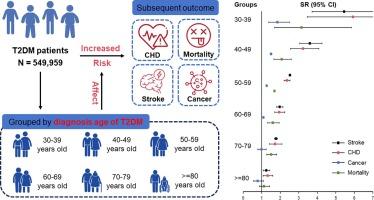
549,959 eligible T2DM patients were included from Ningbo and Jinhua city in Zhejiang province, China. Standardized ratio was used to evaluate the risks of coronary heart disease (CHD), stroke, cancer and all-cause death in different T2DM diagnosis age groups.
Results
For all adverse outcomes, higher excess risks were observed in the youngest age group (30–39) than in the oldest age group (≥80) with T2DM. The standardized incidence ratios (SIR) were 5.93 (95% CI: 3.46, 10.14) for CHD, 5.45 (95% CI: 3.72, 7.99) for stroke and 1.85 (95% CI: 1.38, 2.49) for cancer in the youngest age group, and were 1.32 (95% CI: 1.08, 1.60) for CHD, 1.25 (95% CI: 1.08, 1.44) for stroke, and 0.78 (95% CI: 0.56, 1.09) for cancer, respectively, in the oldest age group. The standardized mortality ratios (SMR) for all-cause death were 3.15 (1.69, 5.84) vs. 1.12 (0.88, 1.43). These excess risks decreased with increasing diagnosis age (all P value < 0.001). Consistent results were observed when individuals were stratified by sex or further excluded with the time from T2DM diagnosis to endpoints less than 1 or 2 years.
Conclusions
Th earlier the diagnosis of T2DM, the higher the risk for subsequent adverse outcomes. It is imperative to enhance the management and monitoring of early-onset patients during follow-up.
确诊 2 型糖尿病时的年龄与心血管疾病、癌症和全因死亡率的发病风险之间的关系:一项基于大型人群队列研究的真实世界研究提供的证据。
目的:研究中国人群中2型糖尿病(T2DM)诊断年龄对后续不良结局的影响。方法:纳入浙江省宁波市和金华市549 959名符合条件的T2DM患者。结果:在所有不良后果中,T2DM 患者的超额风险越高,其不良后果越严重:结果:在所有不良后果中,T2DM 患者中最年轻年龄组(30-39 岁)的超额风险高于最年长年龄组(≥80 岁)。在最年轻的年龄组中,冠心病的标准化发病率(SIR)为 5.93 (95% CI: 3.46, 10.14),中风为 5.45 (95% CI: 3.72, 7.99),癌症为 1.85 (95% CI: 1.38, 2.49)。在最年长的年龄组中,冠心病、中风和癌症的标准化死亡率分别为 1.32(95% CI:1.08,1.60)、1.25(95% CI:1.08,1.44)和 0.78(95% CI:0.56,1.09)。全因死亡的标准化死亡率(SMR)为 3.15 (1.69, 5.84) vs. 1.12 (0.88, 1.43)。这些超额风险随着诊断年龄的增加而降低(均为 P 值):T2DM 诊断越早,随后出现不良后果的风险越高。在随访过程中加强对早发患者的管理和监测势在必行。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Diabetes research and clinical practice
医学-内分泌学与代谢
CiteScore
10.30
自引率
3.90%
发文量
862
审稿时长
32 days
期刊介绍:
Diabetes Research and Clinical Practice is an international journal for health-care providers and clinically oriented researchers that publishes high-quality original research articles and expert reviews in diabetes and related areas. The role of the journal is to provide a venue for dissemination of knowledge and discussion of topics related to diabetes clinical research and patient care. Topics of focus include translational science, genetics, immunology, nutrition, psychosocial research, epidemiology, prevention, socio-economic research, complications, new treatments, technologies and therapy.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


