Prevalence and significance of pulmonary hypertension among hospitalized patients with left heart disease
IF 3.5
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
Abstract
Background
Pulmonary hypertension associated with left heart disease (PH-LHD) prevalence ranges significantly across studies with limited real-world evidence.
Objectives
To investigate the prevalence and prognostic influence of PH-LHD in a nationwide sample.
Methods
Using the 2018 US Nationwide Inpatient Sample we calculated the prevalence of PH across heart failure (HF), cardiomyopathies, aortic, and mitral valve disease. We used logistic regression to assess the impact of PH on LHD and to find significant contributors to in-hospital mortality in the PH-LHD population.
Results
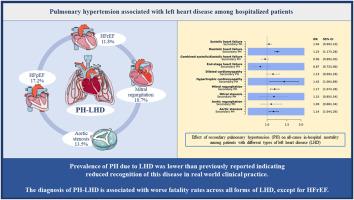
Among 6,270,625 hospitalizations with LHD, 801,535 (12.8 %) had a secondary PH diagnosis. PH-LHD prevalence was 17.2 % in HF with preserved ejection fraction (HFpEF), 11.8 % in HF with reduced ejection fraction (HFrEF), 16.8 % in dilated cardiomyopathy, 12.6 % in hypertrophic cardiomyopathy, 18.7 % in mitral regurgitation, 28.5 % in mitral stenosis, 13.5 % in aortic stenosis, and 13.9 % in aortic regurgitation. PH was associated with increased in-hospital mortality in HFpEF (OR 1.23; 95%CI 1.17–1.28), hypertrophic cardiomyopathy (1.42; 1.06–1.89), mitral regurgitation (1.17; 1.07–1.28), and aortic stenosis (1.14; 1.04–1.26), but not in HFrEF (1.04; 0.99–1.10), or dilated cardiomyopathy (1.13; 0.99–1.29). Among PH-LHD, in-hospital mortality was associated with age, atrial fibrillation/flutter, cancer, and acute cardiac (acute right HF, myocardial infarction, ventricular arrhythmia), or extra-cardiac (stroke, sepsis, pneumonia, acute renal failure, venous thromboembolism) diagnoses.
Conclusion
In a nationwide inpatient analysis the prevalence of PH-LHD was lower than previously reported indicating reduced recognition of this disease in real world clinical practice. The diagnosis of PH-LHD was associated with worse fatality rates across all forms of LHD, except for HFrEF.
左心疾病住院患者肺动脉高压的发病率和意义
背景与左心疾病相关的肺动脉高压(PH-LHD)患病率在不同研究中差异显著,而现实世界中的证据却很有限.目的调查全国样本中PH-LHD的患病率和对预后的影响.方法利用2018年美国全国住院患者样本,我们计算了心力衰竭(HF)、心肌病、主动脉瓣和二尖瓣疾病中PH的患病率。我们使用逻辑回归评估 PH 对 LHD 的影响,并在 PH-LHD 患者中寻找导致院内死亡率的重要因素。结果在 6,270,625 例因 LHD 住院的患者中,有 801,535 例(12.8%)继发 PH 诊断。PH-LHD发病率在射血分数保留型心房颤动(HFpEF)中占17.2%,在射血分数降低型心房颤动(HFrEF)中占11.8%,在扩张型心肌病中占16.8%,在肥厚型心肌病中占12.6%,在二尖瓣反流中占18.7%,在二尖瓣狭窄中占28.5%,在主动脉狭窄中占13.5%,在主动脉反流中占13.9%。PH与HFpEF(OR 1.23;95%CI 1.17-1.28)、肥厚型心肌病(1.42;1.06-1.89)、二尖瓣反流(1.17;1.07-1.28)和主动脉瓣狭窄(1.14;1.04-1.26)的院内死亡率增加有关,但与HFrEF(1.04;0.99-1.10)或扩张型心肌病(1.13;0.99-1.29)无关。在 PH-LHD 患者中,院内死亡率与年龄、心房颤动/扑动、癌症、急性心脏病(急性右侧高频、心肌梗死、室性心律失常)或心脏病外诊断(中风、败血症、肺炎、急性肾功能衰竭、静脉血栓栓塞)有关。在所有形式的 LHD 中,除 HFrEF 外,PH-LHD 诊断与更低的死亡率相关。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Respiratory medicine
医学-呼吸系统
CiteScore
7.50
自引率
0.00%
发文量
199
审稿时长
38 days
期刊介绍:
Respiratory Medicine is an internationally-renowned journal devoted to the rapid publication of clinically-relevant respiratory medicine research. It combines cutting-edge original research with state-of-the-art reviews dealing with all aspects of respiratory diseases and therapeutic interventions. Topics include adult and paediatric medicine, epidemiology, immunology and cell biology, physiology, occupational disorders, and the role of allergens and pollutants.
Respiratory Medicine is increasingly the journal of choice for publication of phased trial work, commenting on effectiveness, dosage and methods of action.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


