Invasive acantholytic anaplastic extramammary Paget disease: A previously unreported neoplasm in the vulva and review of the literature
IF 1.2
Q3 OBSTETRICS & GYNECOLOGY
引用次数: 0
Abstract
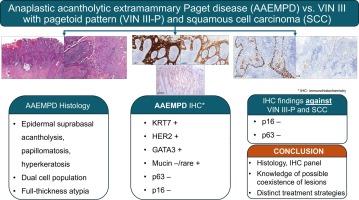
This report describes the first documented invasive acantholytic anaplastic extramammary Paget disease (AAEMPD) of the vulva. An 87-year-old female presented with a recurrent vulvar lesion refractory to topical imiquimod and treated with multiple wide local excisions (WLE). Microscopic examination of the final WLE specimen revealed unique histologic features, primarily supra-basal intraepidermal acantholysis with epidermal papillomatosis and hyperkeratosis. The epidermis, composed of two distinct cell populations, exhibited full-thickness atypia. Paget cells with high mitotic activity were present in the basal and parabasal layers surrounding benign squamous cells in the mid-squamous mucosa. The histologic features were suspicious of the EMPD involving a warty lesion and/or invasive squamous cell carcinoma. In addition to the intraepidermal component, dermal invasion was also present with lymphovascular space invasion. Immunohistochemical studies (KRT7, HER2, and GATA3 reactivity in Paget cells, p63 negativity, and rare mucin in Paget cells) supported the diagnosis of acantholytic anaplastic EMPD. AAEMPD, a rare variant of EMPD, shares similar prognosis and behavior with the classic Paget disease. Recognition and accurate diagnosis of this subtype is crucial for optimal patient management, given distinct treatment strategies compared with other entities in the differential diagnosis.
侵袭性棘皮溶解性无性乳腺外Paget病:一种以前从未报道过的外阴肿瘤及文献综述
本报告描述了首例有记录的外阴侵袭性棘皮溶解性无弹性乳腺外Paget病(AAEMPD)。一位87岁的女性因外阴复发性病变而就诊,外用咪喹莫特(imiquimod)治疗无效,她接受了多次大范围局部切除(WLE)治疗。对最终的 WLE 标本进行显微镜检查后发现了独特的组织学特征,主要是基底层表皮内棘层溶解,伴有表皮乳头状瘤病和角化过度。表皮由两个不同的细胞群组成,呈现全厚不典型性。基底层和副基底层出现了有丝分裂活性很高的 Paget 细胞,围绕着鳞状粘膜中层的良性鳞状细胞。组织学特征显示,EMPD疑似疣状病变和/或浸润性鳞状细胞癌。除表皮内成分外,真皮层也有淋巴管间隙侵犯。免疫组化研究(Paget 细胞中的 KRT7、HER2 和 GATA3 反应性、p63 阴性和 Paget 细胞中罕见的粘蛋白)支持棘溶性无性 EMPD 的诊断。AAEMPD是EMPD的一种罕见变异型,其预后和行为与典型的Paget病相似。与鉴别诊断中的其他实体相比,该亚型的治疗策略有所不同,因此识别和准确诊断该亚型对于优化患者管理至关重要。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Gynecologic Oncology Reports
OBSTETRICS & GYNECOLOGY-
CiteScore
2.00
自引率
0.00%
发文量
183
审稿时长
41 days
期刊介绍:
Gynecologic Oncology Reports is an online-only, open access journal devoted to the rapid publication of narrative review articles, survey articles, case reports, case series, letters to the editor regarding previously published manuscripts and other short communications in the field of gynecologic oncology. The journal will consider papers that concern tumors of the female reproductive tract, with originality, quality, and clarity the chief criteria of acceptance.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


