Lupus nephritis-related chronic kidney disease
IF 29.4
1区 医学
Q1 RHEUMATOLOGY
引用次数: 0
Abstract
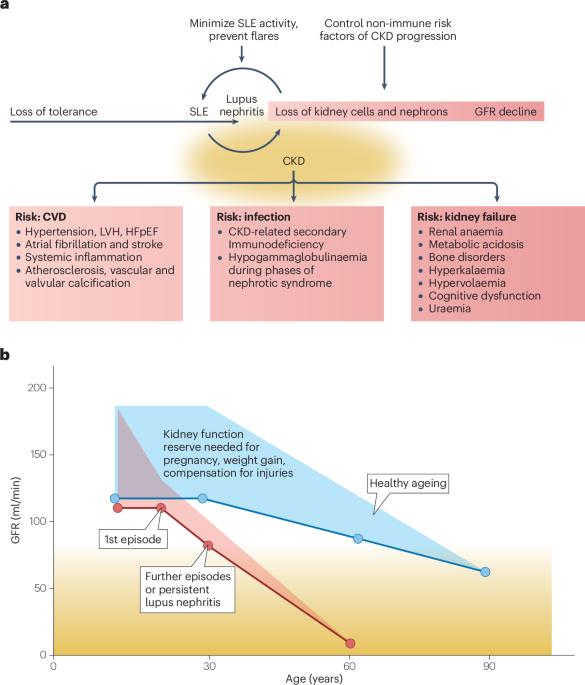
Lupus nephritis is a common complication of systemic lupus erythematosus (SLE) and a determinant of overall morbidity and mortality, as lupus nephritis-related chronic kidney disease (CKD) drives cardiovascular disease and secondary immunodeficiency. Two lines of action are required to prevent the progression of lupus nephritis-related CKD: suppression of autoimmune SLE activity, which is a risk factor for immunopathology-related irreversible kidney injury, and management of non-immune risk factors that contribute to CKD progression. As each episode or relapse of active lupus nephritis implicates CKD progression, preventing flares of lupus nephritis is a key treatment target. Non-immune risk factors of CKD mostly include causes of nephron hyperfiltration, such as obesity, hypertension, sodium- or protein-rich diets and type 2 diabetes mellitus, as well as pregnancy. Nephrotoxic agents and smoking also drive kidney cell loss. Intrinsic risk factors for CKD progression include poor nephron endowment because of prematurity at birth, nephropathic genetic variants, ageing, male sex and previous or concomitant kidney diseases. Care for lupus nephritis involves the control of all modifiable risk factors of CKD progression. In addition, remnant nephron overload can be reduced using early dual therapy with inhibitors of the renin–angiotensin system and sodium–glucose transporter-2, whereas further renoprotective drug interventions are underway. As patients with lupus nephritis are at risk of CKD progression, they would all benefit from interdisciplinary care to minimize the risk of kidney failure, cardiovascular disease and infections. Each episode of lupus nephritis causes irreversible kidney injury, initiating and, subsequently, exacerbating chronic kidney disease. This Review discusses how interdisciplinary care that considers all immune and non-immune risk factors for chronic kidney disease progression can benefit patients with lupus nephritis.

狼疮肾炎相关慢性肾病
狼疮性肾炎是系统性红斑狼疮(SLE)的常见并发症,也是总体发病率和死亡率的决定因素,因为狼疮性肾炎相关慢性肾病(CKD)会引发心血管疾病和继发性免疫缺陷。预防狼疮肾炎相关慢性肾脏病的进展需要采取两条行动路线:一是抑制自身免疫性系统性红斑狼疮的活动,这是导致免疫病理相关不可逆肾损伤的风险因素;二是控制导致慢性肾脏病进展的非免疫性风险因素。由于活动性狼疮肾炎的每次发作或复发都牵涉到慢性肾脏病的进展,因此预防狼疮肾炎复发是治疗的关键目标。慢性肾脏病的非免疫性危险因素主要包括导致肾小球高滤过的原因,如肥胖、高血压、高钠或高蛋白饮食、2 型糖尿病以及妊娠。肾毒性药物和吸烟也会导致肾细胞丢失。导致慢性肾脏病恶化的内在风险因素包括出生时早产、肾脏病理基因变异、年龄增长、男性以及既往或合并肾脏疾病导致的肾小球禀赋差。狼疮性肾炎的治疗包括控制所有可改变的导致慢性肾功能衰竭进展的危险因素。此外,使用肾素-血管紧张素系统抑制剂和钠-葡萄糖转运体-2抑制剂的早期双重疗法可以减轻残余肾小球的超负荷,而进一步的肾保护药物干预正在进行中。由于狼疮性肾炎患者面临着慢性肾功能衰竭恶化的风险,他们都将受益于跨学科护理,以最大限度地降低肾衰竭、心血管疾病和感染的风险。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Nature Reviews Rheumatology
医学-风湿病学
CiteScore
29.90
自引率
0.90%
发文量
137
审稿时长
6-12 weeks
期刊介绍:
Nature Reviews Rheumatology is part of the Nature Reviews portfolio of journals. The journal scope covers the entire spectrum of rheumatology research. We ensure that our articles are accessible to the widest possible audience.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


