Effects of Glucagon-Like Peptide-1 Receptor Agonist on Bone Mineral Density and Bone Turnover Markers: A Meta-Analysis
Abstract
Aims
Glucagon-like peptide-1 receptor agonist (GLP-1RA) may promote bone formation, but conversely, they could also weaken bones due to the reduction in mechanical load associated with weight loss. However, the clinical effects in humans have not been clearly demonstrated. This meta-analysis aimed to evaluate whether GLP-1RAs affect BMD and bone turnover markers.
Material and Methods
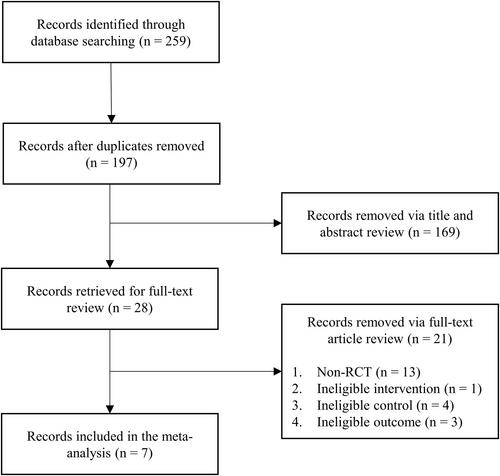
PubMed, Embase, and Scopus were searched on June 13, 2024. The eligibility criteria were: (1) human studies, (2) receiving a GLP-1RA for more than 4 weeks, (3) an untreated control group or a placebo group, (4) reporting of at least one BMD or bone turnover marker, and (5) an RCT design. The risk of bias was assessed using the Cochrane risk of bias 2 tool. Fixed- or random-effects meta-analysis was performed according to heterogeneity.
Results
Seven studies were included in the meta-analysis. GLP-1RAs did not significantly change BMD in the femoral neck (mean difference [MD], 0.01 g/cm2; 95% CI, −0.01–0.04 g/cm2), in the total hip (MD, −0.01 g/cm2; 95% CI, −0.02–0.01 g/cm2), and in the lumbar spine (MD, 0 g/cm2; 95% CI, −0.02–0.02 g/cm2). C-terminal telopeptide of type 1 collagen (CTX), a bone resorption marker, significantly increased after GLP-1RA treatment (MD, 0.04 μg/L; 95% CI, 0.01–0.07 μg/L). GLP-1RAs did not significantly change bone formation markers such as procollagen type 1 N-terminal propeptide, bone-specific alkaline phosphatase, osteocalcin.
Conclusions
GLP-1RA did not affect BMD and bone formation markers. However, GLP-1RAs led to a significant increase in CTX.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


