Prospective cohort study of rotational thromboelastometry in established biliary obstruction: dispelling the myth of auto-anticoagulation
IF 2.7
3区 医学
Q2 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background
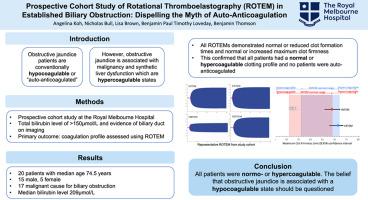
Patients with obstructive jaundice are conventionally described as hypocoagulable due to vitamin K malabsorption. However, associated underlying malignancy and synthetic liver dysfunction are mediators of hypercoagulability. The actual effect of biliary obstruction on the coagulation profile is not well characterised. This study aimed to define the coagulation status of patients with established biliary obstruction using rotational thromboelastometry (ROTEM).
Methods
This prospective cohort study, conducted in an Australian metropolitan hospital, included patients with a total bilirubin level of >150 umol/L and biliary obstruction on imaging. The primary outcome was the coagulation profile assessed using ROTEM.
Results
20 patients were included (median age 74.5 years), 15 were male and 17 had a malignant cause for biliary obstruction. The median bilirubin level was 209 umol/L (IQR: 175.0 umol/L – 255.8 umol/L). On ROTEM, all patients had normal or reduced clot formation times, and normal or increased maximum clot firmness. This confirmed all patients had a normal or hypercoagulable clotting profile, and none were auto-anticoagulated. Vitamin K administration before ROTEM did not vary the coagulation profile.
Discussion
Patients with established biliary obstruction and jaundice, predominantly due to malignancy, were normo or hypercoagulable. The belief that obstructive jaundice is associated with a hypocoagulable state should be questioned.
对胆道梗阻患者进行旋转血栓弹性测量的前瞻性队列研究:打破自动抗凝的神话
阻塞性黄疸患者通常被描述为因维生素 K 吸收不良而导致的低凝状态。然而,相关的潜在恶性肿瘤和合成性肝功能障碍是高凝状态的介质。胆道梗阻对凝血功能的实际影响尚不明确。本研究旨在使用旋转血栓弹性测定法(ROTEM)确定已确诊胆道梗阻患者的凝血状态。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Hpb
GASTROENTEROLOGY & HEPATOLOGY-SURGERY
CiteScore
5.60
自引率
3.40%
发文量
244
审稿时长
57 days
期刊介绍:
HPB is an international forum for clinical, scientific and educational communication.
Twelve issues a year bring the reader leading articles, expert reviews, original articles, images, editorials, and reader correspondence encompassing all aspects of benign and malignant hepatobiliary disease and its management. HPB features relevant aspects of clinical and translational research and practice.
Specific areas of interest include HPB diseases encountered globally by clinical practitioners in this specialist field of gastrointestinal surgery. The journal addresses the challenges faced in the management of cancer involving the liver, biliary system and pancreas. While surgical oncology represents a large part of HPB practice, submission of manuscripts relating to liver and pancreas transplantation, the treatment of benign conditions such as acute and chronic pancreatitis, and those relating to hepatobiliary infection and inflammation are also welcomed. There will be a focus on developing a multidisciplinary approach to diagnosis and treatment with endoscopic and laparoscopic approaches, radiological interventions and surgical techniques being strongly represented. HPB welcomes submission of manuscripts in all these areas and in scientific focused research that has clear clinical relevance to HPB surgical practice.
HPB aims to help its readers - surgeons, physicians, radiologists and basic scientists - to develop their knowledge and practice. HPB will be of interest to specialists involved in the management of hepatobiliary and pancreatic disease however will also inform those working in related fields.
Abstracted and Indexed in:
MEDLINE®
EMBASE
PubMed
Science Citation Index Expanded
Academic Search (EBSCO)
HPB is owned by the International Hepato-Pancreato-Biliary Association (IHPBA) and is also the official Journal of the American Hepato-Pancreato-Biliary Association (AHPBA), the Asian-Pacific Hepato Pancreatic Biliary Association (A-PHPBA) and the European-African Hepato-Pancreatic Biliary Association (E-AHPBA).
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


