Exploring the Relationship Between Somatisation, Facial Pain and Psychological Distress in East Asian Temporomandibular Disorder Patients
Abstract
Objectives
The relationship of somatisation with facial pain duration/intensity, pain-related interference/disability and psychological distress was investigated in East Asian temporomandibular disorder (TMD) patients. Correlations between somatisation, facial pain and psychological characteristics were also explored alongside the demographic/physical factors associated with moderate-to-severe depression and anxiety.
Methods
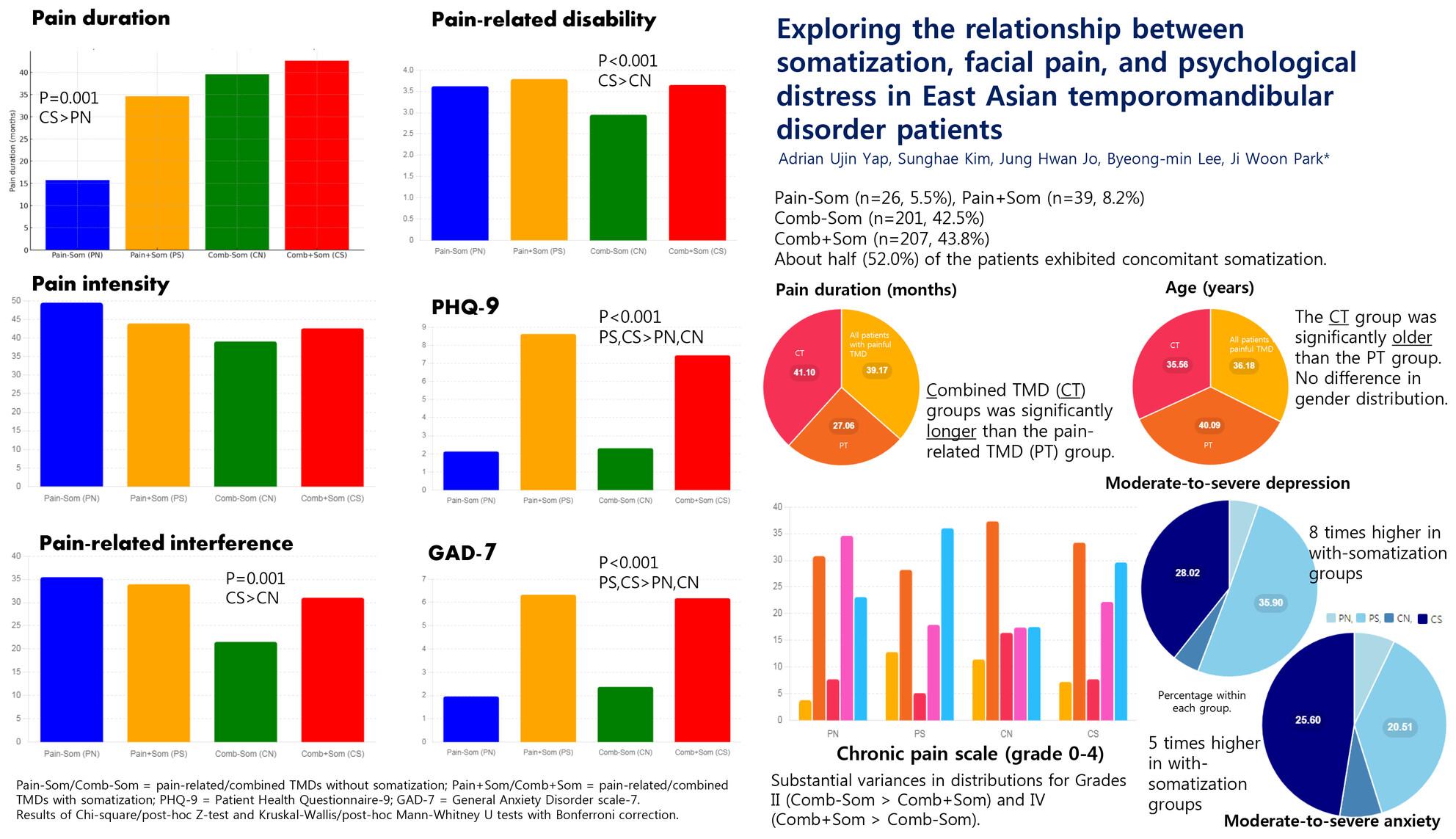
Anonymised data were acquired from records of consecutive ‘first-time’ patients seeking TMD care at a tertiary oral medicine clinic. Axis I physical TMD diagnoses were established utilising the diagnostic criteria for TMDs (DC/TMD) protocol and patients with TMD pain were stratified into those with pain-related (PT) and combined (CT) conditions. Axis II measures administered encompassed the Patient Health Questionnaire-15 (PHQ-15), Graded Chronic Pain Scale (GCPS), Patient Health Questionnaire-9 (PHQ-9) and General Anxiety Disorder Scale-7 (GAD-7). Individuals with PT and CT were further categorised into those without (Pain − Som/Comb − Som) and with somatisation (Pain + Som/Comb + Som). Statistical evaluations were performed with nonparametric and logistic regression analyses (α = 0.05).
Results
The final sample comprised 473 patients (mean age 36.2 ± 14.8 years; 68.9% women), of which 52.0% had concomitant somatisation. Significant differences in pain duration (Comb + Som > Pain − Som), pain-related interference/disability (Comb + Som > Comb − Som) and depression/anxiety (Pain + Som, Comb + Som > Pain − Som, Comb − Som) were discerned. Depression/anxiety was moderately correlated with somatisation (rs = 0.64/0.52) but not facial pain characteristics. Multivariate modelling revealed that somatisation was significantly associated with the prospects of moderate-to-severe depression (OR 1.35) and anxiety (OR 1.24).
Conclusion
Somatisation exhibited a strong association with psychological distress when contrasted with facial pain in East Asian TMD patients.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


