Primary site surgical resection in cM1 oral cavity squamous cell carcinoma
Abstract
Objective
To investigate primary site surgical resection and overall survival (OS) in clinically distantly metastatic (cM1) oral cavity squamous cell carcinoma (OCSCC).
Methods
The 2006–2018 National Cancer Database was queried for patients presenting with cM1 OCSCC who underwent chemotherapy. Binary logistic, Kaplan–Meier, and multivariable Cox proportional hazards regression models were implemented.
Results
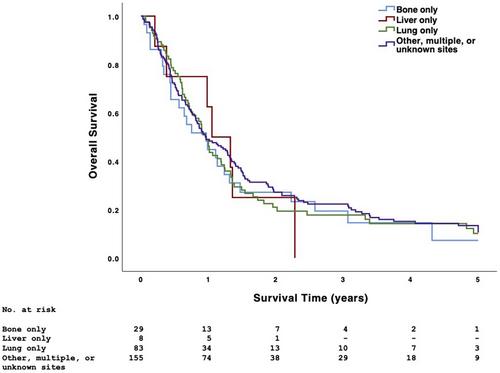
Of 278 patients satisfying inclusion criteria, 139 (50.0%) underwent chemotherapy alone, 80 (28.8%) underwent chemoradiotherapy, 25 (9.0%) underwent surgical resection + adjuvant chemotherapy, and 34 (12.2%) underwent surgical resection + adjuvant chemoradiotherapy; 5-year OS was 9.4%, 15.2%, 8.3%, and 23.8%, respectively (p < .001). Compared with those not undergoing surgical resection, patients undergoing surgical resection underwent radiotherapy more frequently (57.6% vs. 36.5%) but multiple-agent chemotherapy less frequently (40.7% vs. 74.4%) (p < .005). Twenty-one (36.2%) patients undergoing surgical resection had positive surgical margins. Academic facility (adjusted odds ratio [aOR] 3.19, 95% CI 1.54–6.62) and Charlson-Deyo comorbidity score ≥1 (aOR 2.82, 95% CI 1.25–6.32, p < .025) were associated with increased odds of undergoing surgical resection. Compared with chemotherapy alone, chemoradiotherapy (adjusted hazard ratio [aHR] 0.56, 95% CI 0.38–0.83) and surgical resection + adjuvant chemoradiotherapy (aHR 0.37, 95% CI 0.21–0.66) were associated with higher OS (p < .005). Immunotherapy (aHR 0.48, 95% CI 0.28–0.81, p = .006) was also independently associated with higher OS.
Conclusion
A minority of patients with cM1 OCSCC underwent primary site surgical resection. Despite the high rate of positive surgical margins, surgical resection + adjuvant chemoradiotherapy was associated with higher OS than chemotherapy alone, chemoradiotherapy, or surgical resection + adjuvant chemotherapy. Definitive local therapy may benefit select patients with cM1 OCSCC.
Level of evidence: 4.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


