Implementation and impact of a surgical dashboard on pediatric tonsillectomy outcomes: A quality improvement study
Abstract
Introduction
In pediatric tonsillectomy management, the consistent tracking of surgical outcomes and adherence to guidelines are vital. This study explores how a surgical dashboard can serve as a tool in research analysis, translating AAO-HNSF guidelines into measurable performance improvements.
Methods
Using a prospective registry from three pediatric hospitals, a Tableau dashboard was constructed to graphically visualize key demographic and postoperative outcomes (including intensive care unit [ICU] utilization, 30-day emergency department (ED) visits, and postoperative bleed rates) in children undergoing tonsillectomy from 2020 to 2024. From the dashboard data, a retrospective cohort study analyzing 6767 tonsillectomies was conducted from January 2, 2020, to June 20, 2023. Patients were categorized into low-risk, OSA-only (by ICD-10 codes), and high-risk groups based on comorbidities. Logistic regression identified factors influencing ED revisits and unplanned nursing calls. Three quality initiatives were assessed: preoperative school absence notes, perioperative dexamethasone recording, and post-tonsillectomy parental education.
Results
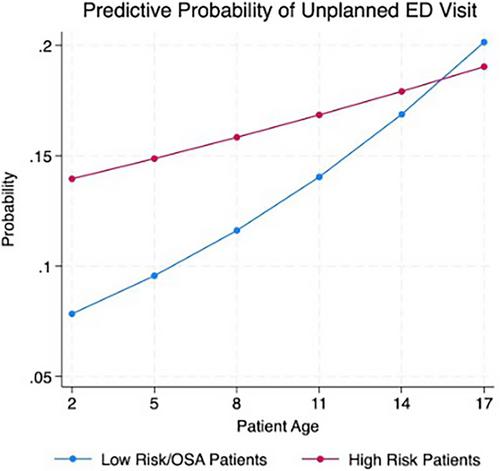
A total of 2122 (31%) were low-risk, 2648 (39%) were OSA-only, and 1997 (30%) high risk. Risk factors that increased the likelihood of ED visits were high-risk comorbidities (OR = 1.46; 95% CI = 1.24–1.74; p < 0.001) and older age (OR = 1.05; 95% CI = 1.03–1.08; p < 0.001). Risk factors that increased the likelihood of an unplanned nursing communication were high-risk comorbidities (OR = 1.53; 95% CI = 1.34–1.75; p < 0.001), older age (OR = 1.03, 95% CI = 1.01–1.04; p = 0.001), and Medicaid insurance (OR = 1.25; 95% CI = 1.09–1.43; p = 0.002). Postoperative bleed control was generally comparable between the groups, at 2.8% (low risk), 2.7% (OSA), 3.2 (high risk) (p = 0.651).
Conclusion
The dashboard aided in data collection, data visualization, and data analysis of quality improvement initiatives, effectively translating guidelines into tangible measures to enhance care.
Level of evidence
NA.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


