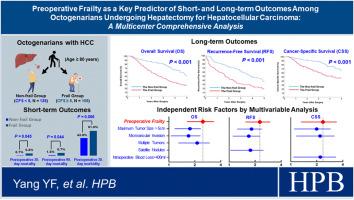
Preoperative frailty as a key predictor of short- and long-term outcomes among octogenarians undergoing hepatectomy for hepatocellular carcinoma: a multicenter comprehensive analysis
IF 2.7
3区 医学
Q2 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
Abstract
Background
When considering hepatectomy for elderly HCC patients, it's essential to assess surgical safety and survival benefits. This study investigated the impact of preoperative frailty, assessed with the Clinical Frailty Scale (CFS), on outcomes for octogenarians undergoing HCC hepatectomy.
Methods
A retrospective cohort study of octogenarians who had hepatectomy for HCC between 2010 and 2022 at 16 hepatobiliary centers was conducted. Patients were categorized as frail or non-frail based on preoperative CFS, with frailty defined as CFS ≥5. The primary endpoints were overall survival (OS), recurrence-free survival (RFS), and cancer-specific survival (CSS), with perioperative outcomes as secondary endpoints.
Results
Among 240 octogenarians, 105 were characterized as being frail. Frail patients had a higher incidence of postoperative 30-day morbidity and postoperative 30-day and 90-day mortality versus non-frail patients. Meanwhile, 5-year OS, RFS and CSS among frail patients were lower compared with non-frail patients. Univariable and multivariable analysis revealed that preoperative frailty was an independent risk factor of postoperative 30-day morbidity (OR: 2.060), OS (HR: 2.384), RFS (HR: 2.190) and CSS (HR: 2.203).
Conclusion
Preoperative frailty, as assessed by the CFS, was strongly associated with both short-term outcomes and long-term survival among octogenarians undergoing hepatectomy for HCC. Incorporating frailty assessment into the preoperative evaluation may help optimize patient selection and perioperative care.
术前虚弱是预测八旬老人肝细胞癌肝切除术短期和长期预后的关键因素:多中心综合分析
在考虑对老年 HCC 患者进行肝切除术时,评估手术安全性和生存益处至关重要。本研究调查了使用临床虚弱量表(CFS)评估的术前虚弱对接受HCC肝切除术的八旬老人预后的影响。该研究对 2010 年至 2022 年期间在 16 个肝胆中心接受 HCC 肝切除术的八旬老人进行了回顾性队列研究。根据术前CFS将患者分为体弱和非体弱,体弱定义为CFS≥5。主要终点为总生存期(OS)、无复发生存期(RFS)和癌症特异性生存期(CSS),围手术期结果为次要终点。在 240 位八旬老人中,有 105 位体弱者。与非体弱患者相比,体弱患者的术后 30 天发病率、术后 30 天和 90 天死亡率较高。同时,与非体弱患者相比,体弱患者的 5 年 OS、RFS 和 CSS 均较低。单变量和多变量分析显示,术前体弱是术后30天发病率(OR:2.060)、OS(HR:2.384)、RFS(HR:2.190)和CSS(HR:2.203)的独立风险因素。在接受 HCC 肝切除术的八旬老人中,由 CFS 评估的术前虚弱程度与短期预后和长期存活率密切相关。将体弱评估纳入术前评估有助于优化患者选择和围手术期护理。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Hpb
GASTROENTEROLOGY & HEPATOLOGY-SURGERY
CiteScore
5.60
自引率
3.40%
发文量
244
审稿时长
57 days
期刊介绍:
HPB is an international forum for clinical, scientific and educational communication.
Twelve issues a year bring the reader leading articles, expert reviews, original articles, images, editorials, and reader correspondence encompassing all aspects of benign and malignant hepatobiliary disease and its management. HPB features relevant aspects of clinical and translational research and practice.
Specific areas of interest include HPB diseases encountered globally by clinical practitioners in this specialist field of gastrointestinal surgery. The journal addresses the challenges faced in the management of cancer involving the liver, biliary system and pancreas. While surgical oncology represents a large part of HPB practice, submission of manuscripts relating to liver and pancreas transplantation, the treatment of benign conditions such as acute and chronic pancreatitis, and those relating to hepatobiliary infection and inflammation are also welcomed. There will be a focus on developing a multidisciplinary approach to diagnosis and treatment with endoscopic and laparoscopic approaches, radiological interventions and surgical techniques being strongly represented. HPB welcomes submission of manuscripts in all these areas and in scientific focused research that has clear clinical relevance to HPB surgical practice.
HPB aims to help its readers - surgeons, physicians, radiologists and basic scientists - to develop their knowledge and practice. HPB will be of interest to specialists involved in the management of hepatobiliary and pancreatic disease however will also inform those working in related fields.
Abstracted and Indexed in:
MEDLINE®
EMBASE
PubMed
Science Citation Index Expanded
Academic Search (EBSCO)
HPB is owned by the International Hepato-Pancreato-Biliary Association (IHPBA) and is also the official Journal of the American Hepato-Pancreato-Biliary Association (AHPBA), the Asian-Pacific Hepato Pancreatic Biliary Association (A-PHPBA) and the European-African Hepato-Pancreatic Biliary Association (E-AHPBA).
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


