Routine beta-blocker therapy after acute coronary syndromes: The end of an era?
Abstract
Background
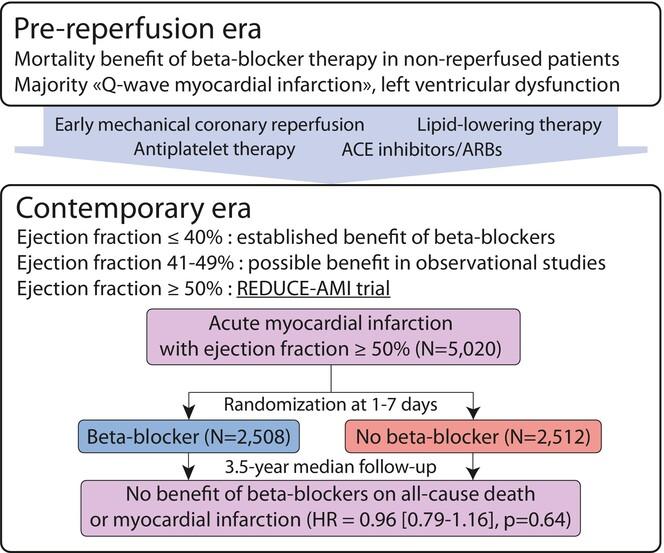
Beta-blocker therapy, a treatment burdened by side effects including fatigue, erectile dysfunction and depression, was shown to reduce mortality and cardiovascular events after acute coronary syndromes (ACS) in the pre-coronary reperfusion era. Potential mechanisms include protection from ventricular arrhythmias, increased ischaemia threshold and prevention of left ventricular (LV) adverse remodelling. With the advent of early mechanical reperfusion and contemporary pharmacologic secondary prevention, the benefit of beta-blockers after ACS in the absence of LV dysfunction has been challenged.
Methods
The present narrative review discusses the contemporary evidence based on searching the PubMed database and references in identified articles.
Results
Recently, the REDUCE-AMI trial—the first adequately powered randomized trial in the reperfusion era to test beta-blocker therapy after myocardial infarction with preserved left ventricular ejection fraction (LVEF)—showed no benefit on the composite of all-cause death or myocardial infarction over a median 3.5-year follow-up. While the benefit of beta-blockers in patients with reduced LVEF remains undisputed, their value in post-ACS patients with mildly reduced systolic function (LVEF 41%–49%) has not been studied in contemporary randomized trials; in this setting, observational studies have suggested a reduction in cardiovascular events with these agents. The adequate duration of beta-blocker therapy remains unknown, but observational data suggests that any mortality benefit may be lost beyond 1–12 months after ACS in patients with LVEF >40%.
Conclusion
We believe that there is sufficient evidence to abandon routine beta-blocker prescription in post-ACS patients with preserved LV systolic function.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


