Diabetes mellitus in stable chronic heart failure and the combination with humoral activation, their association, and prediction of 2-year adverse outcomes. Data from the FAR NHL registry
Abstract
Background/Aim
The study aims to describe the role of diabetes in patients with heart failure.
Methods
In all, 1052 chronic heart failure patients were included in the FARmacology and NeuroHumoral Activation (FAR NHL) multicenter prospective registry. They had ejection fraction below 50% and were on stable medication for at least 1 month.
Results
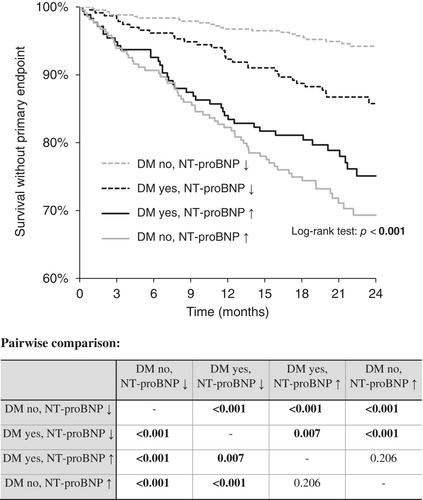
More than one-third (38.9%) of the patients had diabetes mellitus (DM). Diabetic patients (N = 409) were older (median 67 vs. 64, p < 0.001), had higher body mass index (BMI) (30 vs. 28 kg/m2, p < 0.001), much more frequently had ischemic heart disease (71 vs. 47%, p < 0.001), hypertension (80 vs. 67%, p < 0.001), dyslipidemia (89 vs. 69%, p < 0.001), worse renal function (estimated glomerular filtration rate [eGFR] median 63 vs. 73 mL/min/1.73 m2, p < 0.001), and higher N-terminal pro-brain natriuretic peptide (NT-proBNP) (median 681 vs. 463 pg/mL, p = 0.003). All-cause death, left ventricle assist device implantation, and orthotopic heart transplantation were set as the combined primary end point, which was present in 15.5% (163 patients) within the 2-year follow-up. In the 2-year follow-up, 81.0% of patients with diabetes survived without a primary end point, while 85.4% of the patients without diabetes survived, the difference being on the verge of statistical significance (p = 0.089). DM is a statistically significant predictor of NT-proBNP value in univariate analysis, but it is not an independent predictor in a multivariate analysis. When the NT-proBNP level was high, the presence of DM did not influence the prognosis.
Conclusion
The combination of diabetes and NT-proBNP levels may better stratify the prognosis of patients with chronic heart failure.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


