From Angiosomal to Bi-Angiosomal and Extra-Angiosomal Pedicled Perforator Flaps: Optimizing the Use of Local Tissues in Abdominal Wall Reconstruction
Abstract
Introduction
The use of free-style and propeller perforator-based flaps has been popularized for the reconstruction of moderate size defects in the trunk and extremities, while their application in the field of abdominal reconstruction is seldom reported. The purpose of this report is to describe the authors experience with the use of pedicled perforator-based flaps in abdominal wall reconstruction, presenting the innovative concept of transition from angiosomal to bi-angiosomal and extra-angiosomal perforator flaps and showing applications of the different flap designs according to the multiple clinical scenarios.
Patients and Methods
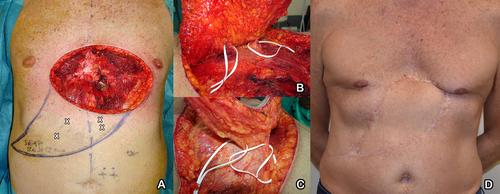
A total of 15 patients underwent abdominal wall reconstruction with angiosomal, bi-angiosomal, and extra-angiosomal pedicled perforator-based flaps harvested from the surrounding abdominal subunits for superficial or full thickness defects of the abdominal wall of moderate and large dimensions. The defects were consequent to soft-tissue sarcomas (STS) and non-melanoma skin cancer (NMSC) resection in 11 and 4 cases, respectively. Operative data, post-operative course, and complications were recorded. Moreover, at 12 months follow-up, patients were asked to rate the esthetic and functional outcomes of the reconstructive procedure on a 5-point Likert scale.
Results
Ten angiosomal perforator flaps (4 DIEP, 4 SCIP, 1 SEAP, and 1 LICAP flaps) and 5 bi-angiosomal and extra-angiosomal conjoined perforator flaps including different vascular territories (3 bilateral DIEP, 1 bilateral SEAP, and 1 ipsilateral DIEP-SEAP flap) were successfully transferred in 15 patients. In two patients, microsurgical anastomoses were performed to guarantee proper vascularization of the additional cutaneous territory. Mean age was 59.3 years. Defect sizes ranged from 98 to 408 cm2 (mean size was 194.7 cm2). Mean operative time was 280 min. Flap surface ranged from 108 to 336 cm2 (mean surface was 209.3 cm2). No major complications were registered. One bi-angiosomal bilateral DIEP flap suffered from partial necrosis and required an additional flap reconstruction. All patients underwent a 12-month follow-up except one, who did not show for clinical follow-up but responded at the Likert scale at clinical follow-up at 9 months. Overall patients' satisfaction was high, with mean esthetic and functional ratings of 4.27 and 3.87.
Conclusion
The use of local tissues is an under-utilized solution in the field of abdominal wall reconstruction. Angiosomal, bi-angiosomal, and extra-angiosomal perforator flaps proved to be a reliable option to provide the transfer of a significant amount of tissue and offer like with like reconstruction while maximizing flap survival.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


